Can seborrheic dermatitis be cured
Seborrheic dermatitis
Diagnosis
To diagnose seborrheic dermatitis, your health care provider will likely talk with you about your symptoms and look at your skin. You may need to have a small piece of skin removed (biopsied) for study in a lab. This test helps rule out other conditions.
Treatment
For adolescents and adults, the main treatments for seborrheic dermatitis are medicated shampoos, creams and lotions. If nonprescription products and self-care habits don't help, your health care provider might suggest that you try one or more of these treatments:
Antifungal gels, creams, lotions, foams or shampoos alternated with another medication. Your health care provider might suggest you try a product with 2% ketoconazole or 1% ciclopirox (Loprox). Or you might rotate between two or more products. Ketoconzole can worsen the dryness of tightly coiled or chemically treated hair and increase the risk of breakage. To ease this effect, use it only once a week with a moisturizing conditioner.
How often you shampoo or apply other antifungal products will depend on your hair-grooming practices and symptoms. Medicated shampoos can be used once a day or 2 to 3 times a week for several weeks. Let the product sit on your scalp for a few minutes see package directions so it has time to work. Then rinse. After your symptoms clear up, use a medicated shampoo just once a week or once every two weeks. This will help prevent a relapse.
Creams, lotions, shampoos or ointments that control inflammation. Your health care provider might prescribe a prescription-strength corticosteroid you apply to the scalp or other affected area. These include hydrocortisone, fluocinolone (Capex, Synalar), clobetasol (Clobex, Temovate) and desonide (Desowen, Desonate). They are effective and easy to use. And use them only until symptoms clear up. If used for many weeks or months without a break, they can cause side effects. These include loss of skin color, thinning skin, and skin showing streaks or lines.
Creams or ointments with a calcineurin inhibitor such as tacrolimus (Protopic) or pimecrolimus (Elidel) may be effective. Another benefit is that they have fewer side effects than corticosteroids do. But they are not first-choice treatments because the Food and Drug Administration has concerns about a possible association with cancer. In addition, tacrolimus and pimecrolimus cost more than mild corticosteroid medications.
- Antifungal medication you take as a pill. If your condition isn't improving with other treatments or is severe, your health care provider may prescribe an antifungal medication in pill form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
ErrorEmail field is required
ErrorInclude a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Lifestyle and home remedies
You may be able to control seborrheic dermatitis with lifestyle changes and home remedies. Many of these are sold in nonprescription forms. You may need to try different products or a combination of products before your condition improves.
The best approach for you depends on your skin type, hair-grooming practices and your symptoms. But even if your condition clears up, it's likely to come back at some point. Watch for the symptoms and resume treating the condition when it recurs. Or use nonprescription antidandruff products in your self-care routine to prevent flare-ups.
Wash your scalp regularly
If regular shampoo doesn't help with dandruff, try nonprescription dandruff shampoos. They are classified according to the active ingredient they contain:
- Pyrithione zinc (DermaZinc, Head & Shoulders, others), also sold as bar soap
- Selenium sulfide (Head & Shoulders, Selsun Blue, others)
- Ketoconazole 1% (Nizoral A-D)
- Tar (Denorex Extra Strength, DHS Tar, others)
- Salicylic acid (Denorex, DHS Sal, others)
How often you shampoo or apply other antifungal products will depend on your hair-grooming practices and symptoms. Medicated shampoos can be used once a day or 2 to 3 times a week for several weeks. After your symptoms clear up, use a medicated shampoo just once a week or once every two weeks. This will help prevent a relapse. Shampoo that contains tar or selenium sulfide can discolor light-colored hair.
Sometimes a shampoo that has helped loses its effectiveness over time. If that's the case, try alternating between two or more types. Be sure to leave your shampoo on for the full recommended time this allows its ingredients to work. Then rinse. These shampoos may be rubbed gently on the face, ears and chest and rinsed off well.
Other home remedies
The following nonprescription treatments and self-care tips may help you control seborrheic dermatitis:
- Soften and remove scales from your hair. Apply mineral oil, peanut oil or olive oil to your scalp. Leave it in for 1 to 3 hours. Then comb or brush your hair and wash it.
- Wash your skin regularly. Use warm, not hot, water and a gentle soap or nonsoap cleanser. Rinse thoroughly. Pat dry and apply a moisturizer while your skin is still damp.
- Apply a medicated cream. First try a mild corticosteroid cream, foam, ointment or oil (Scalpicin Scalp Itch) on affected areas, keeping it away from the eyes. If that doesn't work, try the antifungal cream ketoconazole.
- Don't use styling products. Stop using hair sprays, gels and other styling products while you're treating the condition.
- Don't use skin and hair products that contain alcohol. These can cause the disease to flare up.
- If you have a beard or mustache, shampoo facial hair regularly. Seborrheic dermatitis can be worse under mustaches and beards. Shampoo with 1% ketoconazole daily until your symptoms improve. Then switch to shampooing once a week or once every two weeks. Or shaving might ease your symptoms.
- Gently clean your eyelids. If your eyelids are inflamed or scaly, wash them each night. Use a few drops of baby shampoo mixed with two capfuls of warm water. Wipe away scales with a cotton swab. Warm, damp cloths pressed to your eyelids also may help.
- Gently wash your baby's scalp. If your infant has mild cradle cap, wash the scalp with a mild baby shampoo once a day. Gently loosen the scales with a cloth or an infant hairbrush before rinsing out the shampoo. If scaling persists, first apply mineral oil or olive oil to the scalp for an hour or two. Cradle cap usually disappears in a few weeks or months.
Alternative medicine
Many alternative therapies, including those listed below, have helped some people manage their seborrheic dermatitis. But evidence for their effectiveness isn't proved. It's always a good idea to check with your health care provider before adding any alternative medicines to your self-care routine.
- Tea tree oil. A shampoo with 5% tea tree oil may be used on the affected area. Some studies suggest that tea tree oil can trigger an allergic reaction.
- Aloe. Apply aloe vera gel to the affected area. Aloe is an ingredient in many products, or you can use it directly from the leaf of an aloe plant.
If you're considering dietary supplements or other alternative therapies, talk with your health care provider about their pros and cons.
Preparing for your appointment
You'll probably first visit your primary care provider. Or you may see a doctor who specializes in the diagnosis and treatment of skin conditions (dermatologist).
Here's some information to help you get ready for your appointment.
What you can do
Before your appointment, list your answers to the following questions:
- What are your symptoms, and when did they start?
- Does anything seem to trigger your symptoms?
- What medications are you taking, including those you take by mouth as well as creams or ointments?
- What treatments have you tried so far? Has anything helped?
What to expect from your doctor
Your health care provider is likely to ask you a few questions. Being ready to answer them may free up time to go over any points you want to spend more time on. Your health care provider might ask:
- What are your symptoms, and when did you first notice them?
- Is this the first time you've had these symptoms, or have you had them before?
- How severe are your symptoms? Are they about the same all the time, getting worse, or sometimes better and sometimes worse?
- Do your symptoms affect your quality of life, including your ability to sleep?
- Have you tried any at-home treatments, such as creams, gels or shampoos?
- How often do you use these treatments?
- Does anything seem to help?
- Does anything seem to make your symptoms worse?
- What medications, vitamins or supplements are you taking?
- Have you been under stress lately or experienced major life changes?
What you can do in the meantime
A nonprescription antifungal cream or anti-itch cream can be helpful. If your scalp is affected, a nonprescription antifungal shampoo, foam or other product may ease your symptoms. Try not to scratch or pick at the affected area. This increases your risk of infection.
Sept. 27, 2022
Can Seborrheic Dermatitis Be Cured? A Closer Look at Treatment Options and Long-Term Management
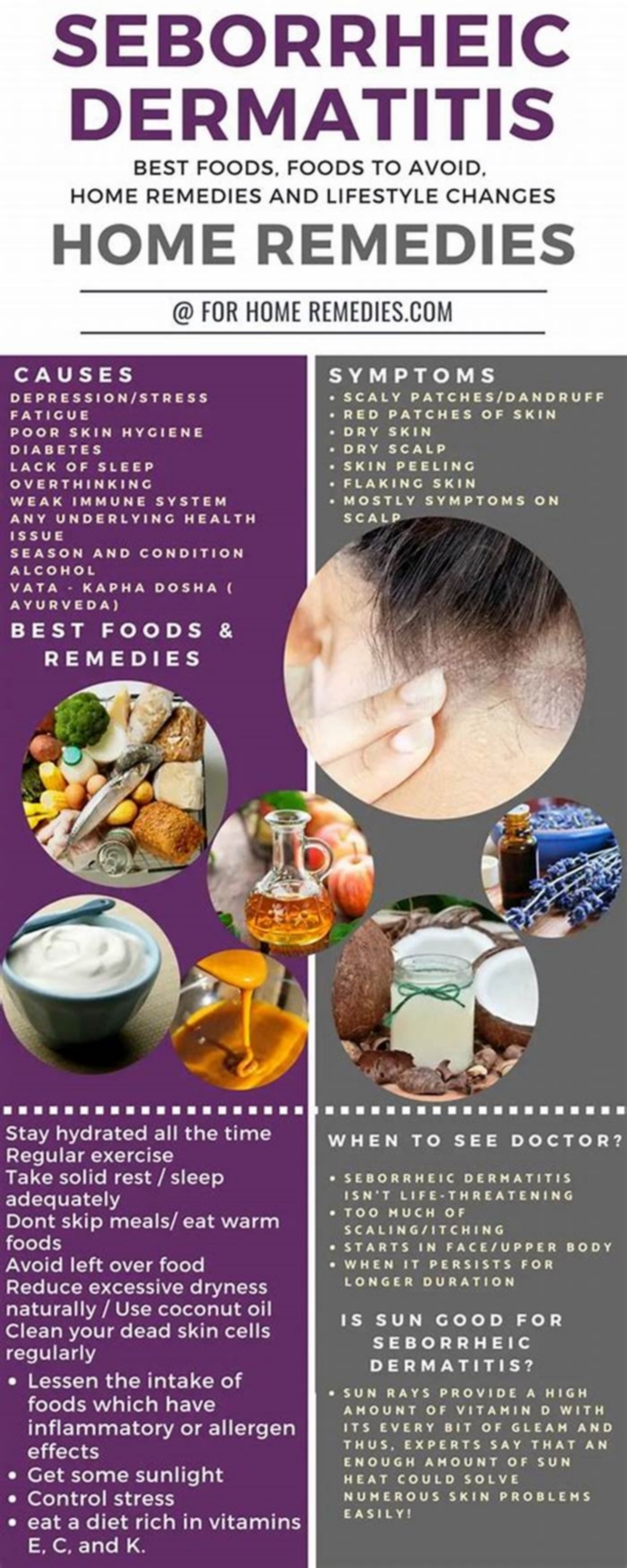
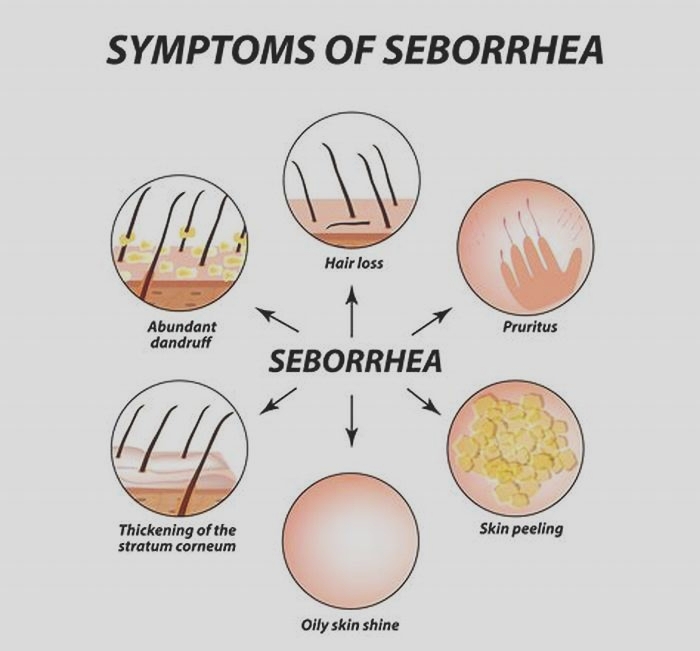
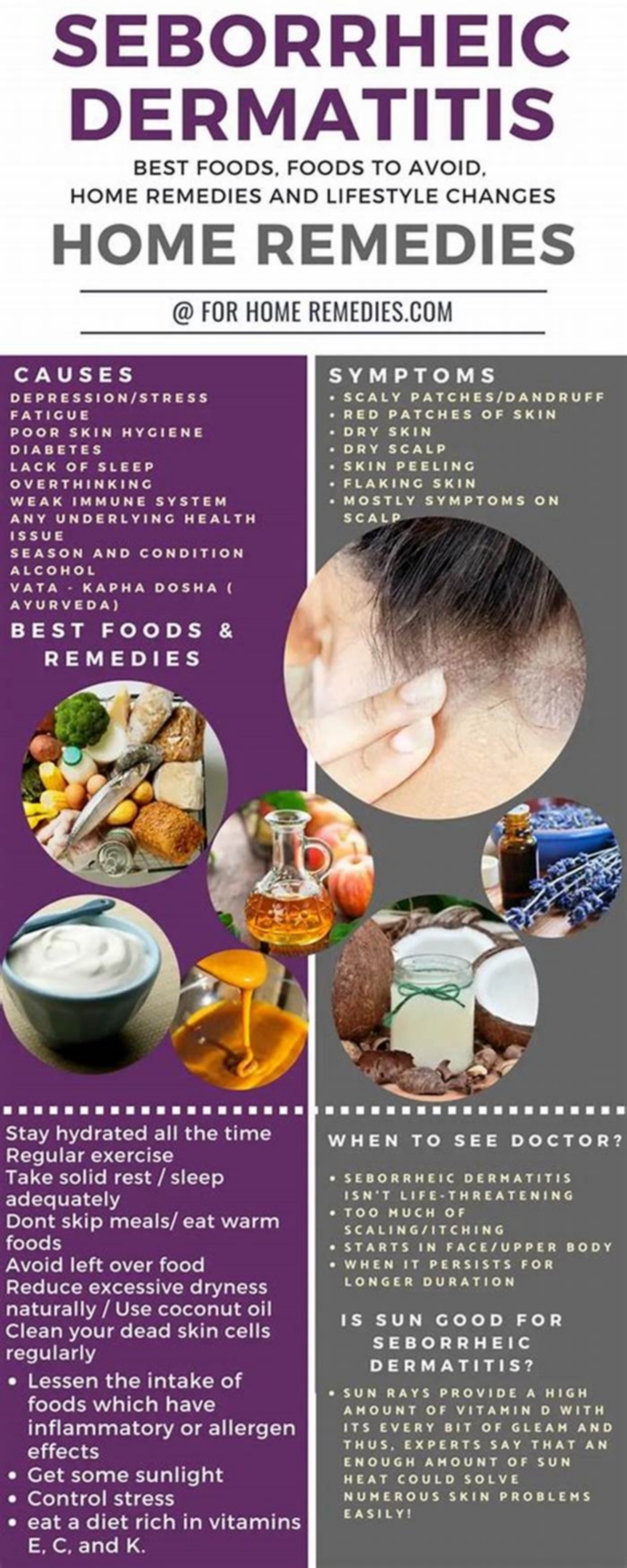
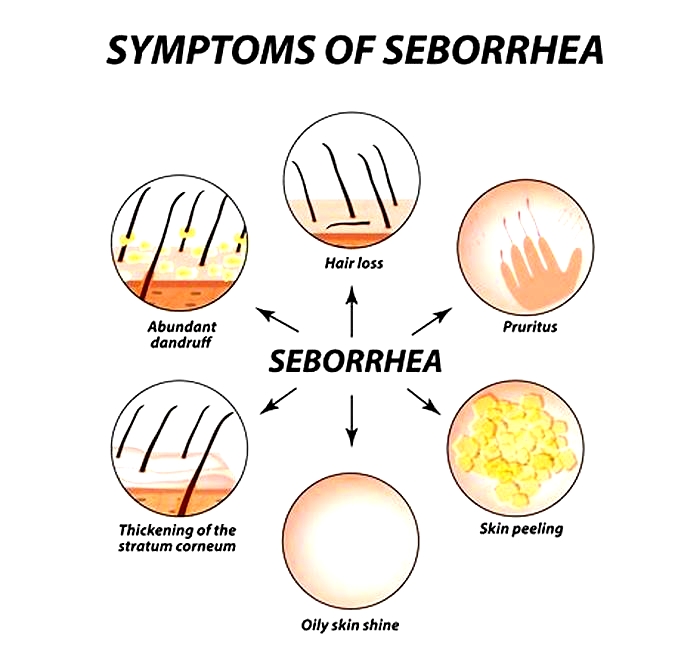
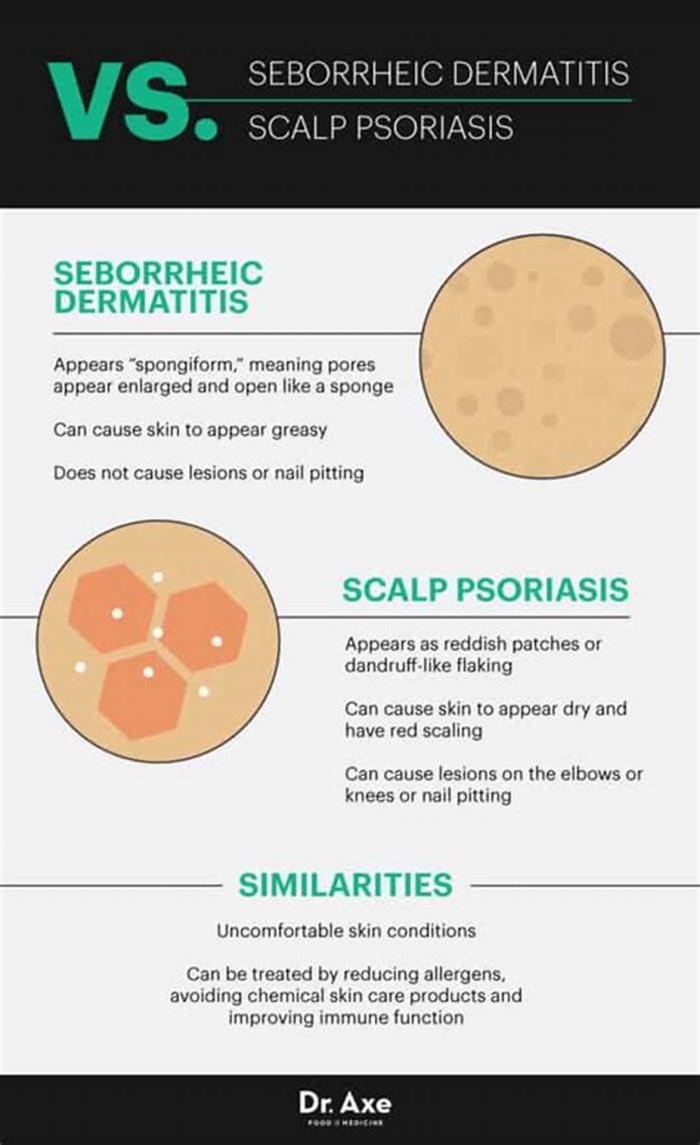
Seborrheic dermatitis, also known as seborrheic eczema, is a common chronic inflammatory skin condition that mainly affects the scalp and face [1]. Characterized by red, flaky, itchy skin and dandruff, seborrheic dermatitis can be distressing and frustrating to deal with.
As a lifelong condition with periodic flare-ups, an obvious question arises can seborrheic dermatitis be cured for good?
The Complex Nature of Chronic Skin Conditions
When it comes to skin disorders like seborrheic dermatitis, the notion of a cure is complex. Unlike acute infections that can be treated and resolved in a short time, chronic diseases involve various biological, psychological, and lifestyle factors [2].
For instance, even when treated successfully, some patients with chronic conditions still perceive themselves as unhealed [3]. Feeling cured encompasses more than just the physical symptoms and requires a holistic outlook.
Furthermore, while treatments can provide symptom relief, they often cannot eliminate the root causes behind complex conditions like seborrheic dermatitis [2]. Ongoing management is needed to maintain remission and prevent flare-ups.
Aiming for Long-Term Remission Through Multi-Targeted Approaches
Given the chronic nature of seborrheic dermatitis, the goal of treatment is typically long-term remission rather than an outright cure [3]. This involves using various therapies to control symptoms and keep flare-ups at bay.
Some key treatment approaches include:
- Topical antifungal agents like ketoconazole to reduce Malassezia yeast overgrowth, a contributor to seborrheic dermatitis [6].
- Topical anti-inflammatory creams containing steroids to calm inflammation [7].
- Antidandruff shampoos with ingredients like selenium sulfide and pyrithione zinc to reduce scalp irritation and flaking [8].
- Immunomodulators like tacrolimus that alter the immune response [1].
Rather than banking on a single miracle cure, using a combination of therapies that target different aspects of the condition is recommended for long-term management [10].
Lifestyle and self-care measures are also important:
- Managing stress levels, which can worsen seborrheic dermatitis [11].
- Avoiding skin irritants like harsh soaps.
- Following a balanced, nutritious diet [4].
With a multi-pronged approach, periods of remission can be extended and flare-ups minimized. While not a permanent cure, long-term symptom control is achievable.
The Psychological Aspects of Living With Chronic Skin Conditions
Aside from physical symptoms, the chronic nature of seborrheic dermatitis also takes a psychological toll anxiety, depression, and lowered self-esteem are common [12].
As symptoms persist for years, patients may feel hopeless and assume they will never be cured. Unrealistic expectations create more frustration when a definitive cure remains elusive.
Therefore, managing chronic skin conditions like seborrheic dermatitis requires addressing both physical and mental health [13]. Being patient and focusing on achievable treatment goals are key for coping psychologically. Support groups can also provide emotional support.
Looking Ahead: Advancing Our Understanding
While current therapies can effectively manage symptoms long-term, there is still room for progress in understanding seborrheic dermatitis. For instance, questions remain about:
- The precise roles of yeasts like Malassezia in causing inflammation [14].
- Why seborrheic dermatitis develops in the first place [15].
- How different treatments like antifungals and steroids work on a molecular level [16].
With continued research, our knowledge can expand to uncover new treatment targets and options. Gene-based therapies may emerge as we unravel the genetic underpinnings of seborrheic dermatitis [17, 18].
For now, a sustained, multi-therapy approach offers the best chance at long-term remission. While seborrheic dermatitis cannot be permanently cured, its impacts can be reduced significantly through diligent management. With the right treatment plan and outlook, living symptom-free for extended periods is an achievable goal.