How do you get rid of fungal skin infection in dogs

Yeast Infections in Dogs
What Are Yeast Infections in Dogs?
Does your dog frantically itch their skin? Have you noticed a bad smell or greasy fur when you pet them?
If so, they may have a yeast infection.
Yeast are fungal organisms that normally live on a dogs skin without causing problems. However, when a dogs immune system weakens or an underlying health condition, such as hypothyroidism, is present, yeast can overgrow and cause an infection.
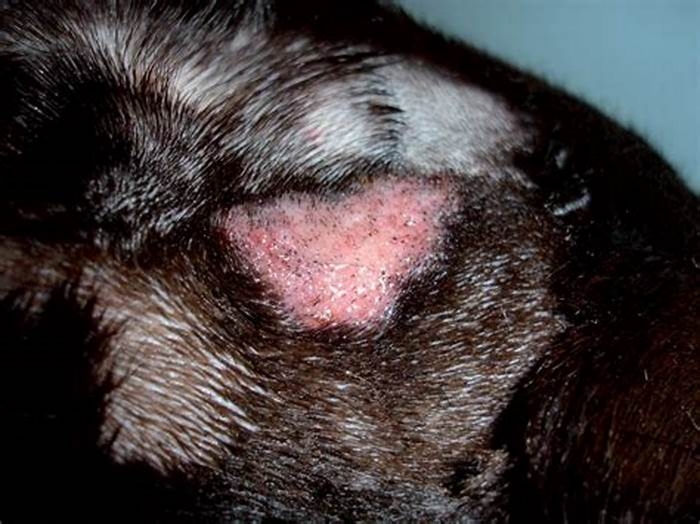
The yeast that commonly causes skin infections in dogs is Malassezia, which grows on warm, moist areas of the skin. Yeast infections cause extreme itchiness and changes to the skin, such as thickening and discoloration over time.
Yeast infections in dogs are common among pups of all ages.
While yeast infections in dogs are not considered medical emergencies, they should be treated by a veterinarian immediately to prevent symptoms from worsening. If left untreated, yeast infections can cause extreme discomfort, which can lead to a decreased appetite and lethargy, necessitating prompt veterinary care.
Because yeast infections typically develop secondary to an underlying illness or suppressed immune system, they are not contagious among dogs or to pet parents.
Types of Yeast Infections in Dogs
Yeast infections can affect various areas of the skin, including the ears, skin folds, paws, armpits, vulva, and groin.
EarsYeast infections of the earalso referred to as yeast otitiscause a thick, brown discharge and strong odor in the ear canal. Affected dogs repeatedly scratch their ears to try to relieve the discomfort. They may also shake their heads and develop a head tilt. Ear infections are commonly related to food allergies.
SkinYeast dermatitis refers to a yeast infection anywhere on the skin. Affected dogs have a musty odor, greasy coat, flaky or thickened skin, and hair loss. They tend to lick the affected areas of the body, which leads to brown discoloration of the skin over time.
Dermatitis, which is often due to allergies or a suppressed immune system, can affecta dogs skin folds, armpits, vulva, and groin.
PawsYeast infections that affect the paws are generally related to environmental allergies, such as allergies to grass or pollen. Dogs constantly chew or lick their itchy paws, which leads to brown discoloration between the paw pads. Over time, open sores can develop on the paws.
Symptoms of Yeast Infections in Dogs
Signs of yeast infections in dogs can vary depending on what area of the body is affected.
Symptoms of yeast otitis may include:
Symptoms of yeast dermatitis may include:
Itchy skin
Small, red bumps on the skin
Brown discoloration of the skin
Frequent licking or chewing of the affected area
Greasy hair coat
Thickened skin
Strong odor
Symptoms of a yeast infection affecting the paws may include:
Licking and chewing the paws
Brown discoloration of the skin and fur
Red, moist areas between the paw pads
Causes of Yeast Infections in Dogs
Yeast is opportunistic, which means that although it is naturally present on the skin, it can cause an infection when conditions are favorable.
Yeast infections in dogs can develop if a pup has a weak immune system or an underlying health condition. Underlying environmental or food allergies can predispose dogs to developing yeast infections.
Skin parasites, including fleas and mites, can cause dogs to repeatedly itch their skin, which disrupts the normal skin barrier, making an infection more likely.
Some breedssuch as Pit Bulls, Boxers, and Cocker Spanielsare more frequently affected by yeast infections.
How Veterinarians Diagnose Yeast Infections in Dogs
A vet may use several tests to diagnose a yeast infections in dogs.
First, they will gather a through medical history, including when the symptoms started, if your pet is taking any medications, and if they have previously been diagnosed with any health conditions.
Next, your veterinarian will perform a full physical exam to check your dogs overall health. They may also perform blood work to check for any abnormalities.
Additional tests will depend on what your veterinarian finds during the initial exam, but may include the following:
Tape impressionDuring this test, your vet presses a piece of clear tape to the affected area of skin to collect a sample. Its then stained and examined under a microscope to identify yeast.
CytologyA cotton swab is used to collect a sample from the affected area, and it is then rubbed gently onto a microscope slide. The sample is then stained and examined under a microscope to look for yeast.
CultureA sterile cotton swab is used to collect a sample from the affected area. It is then sent to a lab to identify the type of organism present.
Skin biopsyFor chronic infections or those that are unresponsive to treatment, a small sample of skin can be taken and sent to a lab for a more accurate diagnosis.
Treatment of Yeast Infections in Dogs
Treatment for yeast infections in dogs will depend on the location and severity of the infection. Yeast dermatitis is often treated with antifungal medications and prescription shampoos.
If the infection affects only one area, a topical medication may be all that is needed. For more widespread infections, oral medications and frequent bathing can help resolve the issue.
Yeast otitis is typically treated with topical antifungal medications and steroids to reduce inflammation. Your veterinarian may recommend that you use a medicated ear wash prior to instilling ear medications.
Paw yeast infections may benefit from medicated antifungal wipes and oral medications, including antifungals and steroids.
Recovery and Management of Yeast Infections in Dogs
Because yeast infections in dogs often develop secondary to another health condition, they will not resolve without veterinary treatment.
Determining the underlying cause of the yeast infection and treating it accordingly improves treatment success. For example, if your dog has an underlying food allergy, an accurate diagnosis and treatment can help their skin improve.
It can take a few weeks to a few months for a yeast infection to fully resolve, depending on the severity. Most dogs start to feel relief from their symptoms in a week or two, but it can take several additional weeks for a pet parent to notice significant improvement to their skin and coat.
Prevention of Yeast Infections in Dogs
Ensuring your dog receives regular preventive care and vaccinations keeps them healthy and less likely to develop infections.
Additionally, health conditions that can lead to yeast infections in dogs can be caught and managed early during routine wellness visits.
Yeast Infections in Dogs FAQs
What food causes yeast infections in dogs?
Most of the food ingredients that cause allergies in dogs are proteins. Chicken is the most common food allergen related to yeast infections.
What happens if dog yeast infections go untreated?
If a dogs yeast infection is left untreated, it will progressively worsen and lead to extreme discomfort. Over time, the discomfort can cause the dog to become very sick.
What should I feed my dog when they have a yeast infection?
Unless the yeast infection is due to an underlying food allergy, its generally fine to continue your dogs usual diet. However, it is best to follow your veterinarians recommendations when deciding what to feed your dog.
Featured Image:SerhiiBobyk/iStock / Getty Images Plus via Getty Images
WRITTEN BY
Brittany Kleszynski, DVMVeterinarian
Dr. Brittany Kleszynski is a veterinarian and freelance medical writer who specializes in creating meaningful content that engages readers...
Everything You Need to Know About Fungal Skin Infections
Many common fungal infections can affect the skin.
Yeast infection (Candida skin infection)
Yeast is a type of fungus.
A yeast called Candida is naturally present on the skin and inside the human body. When it overgrows, an infection can occur, including on the skin. The most common species of Candida is Candida albicans.
Other names for a yeast infection of the skin include:
The infection occurs in warm, moist, and poorly ventilated areas. Areas that are typically infected include the folds of the buttocks (as in certain types of diaper rash) and under the breasts.
The symptoms of a yeast infection of the skin can include:
Other yeast infectionsThe mucous membranes are another common site of fungal infections. Some examples of yeast infections in the mucous membranes are vaginal yeast infections and oral thrush.
How its diagnosed
A primary care doctor should be able to diagnose a yeast infection of the skin during a physical examination. They may also swab the skin and use a skin culture to confirm that yeast is the organism causing your symptoms.
If you see a dermatologist instead, they may perform a skin scraping of the rash and then view the sample under a microscope to determine if theres Candida growth.
How its treated
An important step in treating any yeast infection is keeping the skin clean and dry.
Some yeast infections will go away on their own. Prescription and over-the-counter (OTC) antifungal drugs are also available. These drugs can either kill fungi directly or prevent them from growing and thriving.
Topical versions include:
- clotrimazole
- econazole
- ketoconazole
- nystatin
- oxiconazole
To help reduce itching, you can also use a corticosteroid cream such as hydrocortisone.
Powders may help you keep your skin dry. Its important to apply them 2 to 3 hours before or after applying any creams.
If the infection doesnt resolve or improve, a doctor may prescribe oral antifungal medications, such as:
To help treat diaper rash, consider using zinc oxide creams to soothe your babys skin. OTC options include products from the brands:
- A+D
- Balmex
- Desitin
- Triple Paste
Home remedies such as changing diapers more frequently and using disposable diapers may also relieve symptoms.
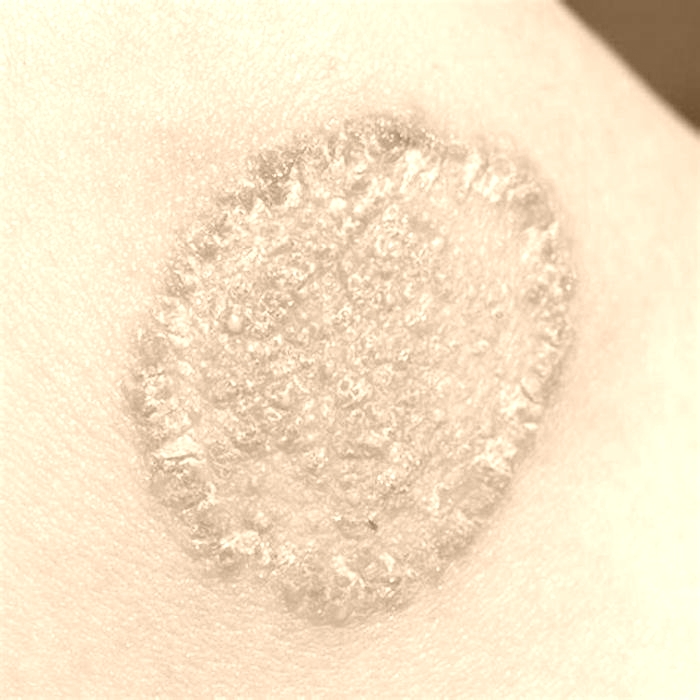
Ringworm of the body (tinea corporis)
Ringworm is a common fungal skin infection. Its highly contagious but not serious.
Despite its name, ringworm is caused by a fungus and not a worm. It typically occurs on the torso and limbs, in a subtype known as ringworm of the body (tinea corporis). Ringworm on other areas of the body can go by different names, such as jock itch and athletes foot.
The main symptom of ringworm is a ring-shaped rash with slightly raised edges. The skin inside these circular rashes usually looks healthy. The rash can spread and is often itchy.
Ringworm can come from petting an animal infected with the fungus or from gyms and gym mats.
How its diagnosed
A doctor can usually diagnose ringworm by sight or after performing a skin scraping.
Some doctors may also perform a fungal culture to help them determine a diagnosis.
How its treated
Ringworm of the body thats limited to a few areas can usually be treated with a topical antifungal medication, such as:
- clotrimazole (Lotrimin AF Ringworm Cream)
- econazole
- ketoconazole (Extina, Ketozole)
- luliconazole (Luzu)
- naftifine
- oxiconazole (Oxistat)
- sulconazole (Exelderm)
- terbinafine (Lamisil AT Cream, Silka Antifungal Cream)
Doctors often recommend oral antifungals for a deeper or more extensive infection. They include:
- fluconazole (Diflucan)
- itraconazole (Sporanox)
- terbinafine
Ringworm of the scalp (tinea capitis)
This fungal infection affects the skin of the scalp and the associated hair shafts. Its most common in children and teens 3 to 14 years old.
You can contract ringworm of the scalp from animals, soil, or other humans (via hairbrushes or hats).
Symptoms of ringworm of the scalp (tinea capitis) can include:
- broken hair shafts
- localized bald patches that may appear scaly or red
- associated scaling and itching
- associated tenderness or pain in the patches
- patches that ooze or crust over
- permanent hair loss, in some severe cases
It may resemble severe dandruff.
It can also cause symptoms unrelated to the scalp, such as fever and swollen lymph nodes in the neck.
How its diagnosed
A doctor can diagnose ringworm of the scalp during a physical examination.
They usually perform a skin scraping, such as a skin lesion KOH exam. In the skin lesion KOH exam, skin scrapings are mixed with potassium hydrochloride (KOH) to determine if fungi are present.
How its treated
Ringworm of the scalp requires prescription oral medication, which may come in the form of a tablet, capsule, or liquid. Examples include:
- fluconazole (Diflucan)
- griseofulvin (Fulvicin, Gris-PEG), which is typically the drug of choice and is safe for children
- itraconazole (Sporanox)
- terbinafine
Everyone with ringworm of the scalp should use an antifungal shampoo. All members of their household should use it too. Examples include ketoconazole shampoo (Nizoral Anti-Dandruff Shampoo).
Jock itch (tinea cruris)
Jock itch happens in the area near your groin and thighs. Its most common in men and adolescent boys.
The main symptom is an itchy, red, and sometimes painful rash that typically starts in the groin or around the upper inner thighs. The rash may worsen after exercise or other physical activity and can spread to the buttocks and abdomen.
The affected skin may also appear:
- scaly
- flaky
- cracked
- moist and possibly macerated, in the case of an open sore
The outer border of the rash can be slightly raised and darker.
How its diagnosed
A doctor can diagnose jock itch during a physical examination or after examining a sample under a microscope.
How its treated
Treatment often begins with OTC or prescription creams.
OTC creams, sprays, and powders include:
- butenafine (Lotrimin Ultra Jock Itch Cream)
- clotrimazole (Lotrimin AF Jock Itch Antifungal Cream)
- miconazole (CareALL Miconazole Cream, Lotrimin AF Jock Itch Antifungal Powder Spray)
- terbinafine (Lamisil AT Cream for Jock Itch, Silka Antifungal Cream, Silka Jock Itch Cream)
Prescription creams include:
- econazole
- ketoconazole (Ketozole)
- luliconazole (Luzu)
- oxiconazole (Oxistat)
- sulconazole (Exelderm)
Applying a cool compress can also help soothe the skin.
If topical treatments dont work, a doctor may prescribe oral antifungals, such as:
- fluconazole (Diflucan)
- itraconazole (Sporanox)
- terbinafine
Oral medications are typically reserved for recurrent, treatment-resistant, or chronic infections.
Tinea versicolor (pityriasis versicolor)
In tinea versicolor, small oval discolored patches develop on the skin. Its sometimes called pityriasis versicolor.
This infection is caused by an overgrowth of a fungus called Malassezia. Malassezia is naturally present on the skin of most adults.
The discolored skin patches mostly occur on the back, chest, and upper arms, but they can also affect the scalp. They may look lighter or darker than the rest of the skin and can be red, pink, tan, or brown. On people with darker skin, the patches may appear white. These patches can be itchy, flaky, or scaly.
Tinea versicolor is more likely to appear during the summer or in areas with a warm, wet climate. Its also common in people who work out or sweat often. The condition can sometimes return following treatment.
How its diagnosed
A doctor can diagnose tinea versicolor with a:
- physical examination
- Woods lamp examination, in which a healthcare professional uses a handheld blacklight to confirm the presence of fungi or bacteria
- skin lesion biopsy, which involves removing a small skin sample and having it tested in a laboratory
- skin lesion KOH exam
How its treated
The standard treatment for tinea versicolor is topical products such as soaps, creams, lotions, and shampoos. Ingredients to look for include:
- ketoconazole, found in products such as prescription-strength shampoo and Extina foam
- pyrithione zinc, found in products such as Vanicream Z-Bar Medicated Cleansing Bar, Vanicream Dandruff Shampoo, and Selsun blue Itchy Dry Scalp Antidandruff Shampoo
- selenium sulfide, found in products such as Selsun blue Moisturizing Antidandruff Shampoo and Selsun blue Medicated Antidandruff Shampoo
If tinea versicolor returns following treatment, a doctor may recommend you use a medicated cleanser once or twice a month.
Oral medication is rarely needed. A doctor may prescribe a short course of oral antifungals if tinea versicolor is recurrent, treatment-resistant, widespread, severe, or creates thick scales.
They include:
- fluconazole (Diflucan)
- itraconazole (Sporanox)
Athletes foot (tinea pedis)
Athletes foot affects the skin on your feet, often between your toes. It can also appear on the soles of your feet.
Typical symptoms of athletes foot include:
- itching or a burning, stinging sensation between your toes or on the soles
- skin that appears red, scaly, dry, or flaky
- peeling skin
- thickened soles
- cracked or blistered skin
- deep blisters on the soles, in rare cases
In some cases, the infection can also spread to other areas. Examples include the:
- nails, as in onychomycosis
- groin, as in jock itch (tinea cruris)
- hands, as in tinea manuum
How its diagnosed
A doctor can diagnose athletes foot by observing your symptoms or performing a skin test such as the skin lesion KOH exam.
How its treated
You can treat athletes foot with a variety of OTC topical products, such as:
- butenafine (Lotrimin Ultra Athletes Foot Cream)
- clotrimazole (CareALL Athletes Foot Cream, Lotrimin AF Cream for Athletes Foot)
- miconazole (Desenex Athletes Foot Shake Powder)
- terbinafine (Lamisil AT Cream, Lamisil AT Cream for Athletes Foot, Silka Antifungal Cream)
- tolnaftate (Dr. Scholls Odor-X Antifungal Spray Powder, Lotrimin AF Athletes Foot Daily Prevention Deodorant Powder Spray, Tinactin Athletes Foot Cream)
Terbinafine tends to be the fastest-acting of these medications.
If OTC products dont help clear up athletes foot within 2 weeks or so, a doctor may prescribe:
- prescription-strength topical clotrimazole
- sulconazole (Exelderm)
Doctors usually prescribe oral antifungals when the infection is recurrent, causes blisters, or involves the tops of the feet, soles, or heels. They include:
- fluconazole (Diflucan)
- griseofulvin (Fulvicin, Gris-PEG), which is safe for children
- itraconazole (Sporanox)
- terbinafine
Did you know?Athletes foot tends to recur, so its important to dry the toes and feet thoroughly after showering or bathing. Use a powder, especially in between the toes.
Onychomycosis
Onychomycosis is a fungal infection of the nails. It can affect the fingernails or the toenails, although infections of the toenails are
Symptoms of onychomycosis include nails that:
How its diagnosed
A doctor will usually take a nail clipping and some subfungal debris and send them off for a periodic acidSchiff (PAS) stain or culture.
On some occasions, they may perform a skin lesion KOH exam. However, the PAS stains and cultures are more accurate.
How its treated
Prescription medications are often required to treat this type of infection. The standard treatment is oral terbinafine. Its typically prescribed for 6 or 12 weeks, depending on whether you have a fingernail or toenail infection.
Treatment is notoriously tricky due to factors such as prolonged treatment time and the likelihood of recurrence.
Other oral antifungals that may be used include:
- fluconazole (Diflucan)
- griseofulvin (Fulvicin, Gris-PEG), which is safe for children
- itraconazole (Sporanox)
Doctors often prescribe topical antifungals as well. They include:
- ciclopirox (Ciclodan)
- efinaconazole (Jublia)
- tavaborole (Kerydin)
In severe cases, a doctor may remove some or all of an affected nail.
Emerging treatment options include lasers and light therapy. More data on their effectiveness is needed.