How long does it take for seborrheic dermatitis to go away

Seborrheic dermatitis: Diagnosis and treatment
 Biosimilars: 14 FAQs
Biosimilars: 14 FAQsFind answers to questions patients ask about this newer treatment option, including, Whats involved in switching from a biologic to a biosimilar?
Featured
 Laser hair removal
Laser hair removalYou can expect permanent results in all but one area. Do you know which one?
 Scar treatment
Scar treatmentIf you want to diminish a noticeable scar, know these 10 things before having laser treatment.
 Botox
BotoxIt can smooth out deep wrinkles and lines, but the results arent permanent. Heres how long botox tends to last.
Featured
 Find a Dermatologist
Find a DermatologistYou can search by location, condition, and procedure to find the dermatologist thats right for you.
 What is a dermatologist?
What is a dermatologist?A dermatologist is a medical doctor who specializes in treating the skin, hair, and nails. Dermatologists care for people of all ages.
Seborrheic dermatitis
Diagnosis
To diagnose seborrheic dermatitis, your health care provider will likely talk with you about your symptoms and look at your skin. You may need to have a small piece of skin removed (biopsied) for study in a lab. This test helps rule out other conditions.
Treatment
For adolescents and adults, the main treatments for seborrheic dermatitis are medicated shampoos, creams and lotions. If nonprescription products and self-care habits don't help, your health care provider might suggest that you try one or more of these treatments:
Antifungal gels, creams, lotions, foams or shampoos alternated with another medication. Your health care provider might suggest you try a product with 2% ketoconazole or 1% ciclopirox (Loprox). Or you might rotate between two or more products. Ketoconzole can worsen the dryness of tightly coiled or chemically treated hair and increase the risk of breakage. To ease this effect, use it only once a week with a moisturizing conditioner.
How often you shampoo or apply other antifungal products will depend on your hair-grooming practices and symptoms. Medicated shampoos can be used once a day or 2 to 3 times a week for several weeks. Let the product sit on your scalp for a few minutes see package directions so it has time to work. Then rinse. After your symptoms clear up, use a medicated shampoo just once a week or once every two weeks. This will help prevent a relapse.
Creams, lotions, shampoos or ointments that control inflammation. Your health care provider might prescribe a prescription-strength corticosteroid you apply to the scalp or other affected area. These include hydrocortisone, fluocinolone (Capex, Synalar), clobetasol (Clobex, Temovate) and desonide (Desowen, Desonate). They are effective and easy to use. And use them only until symptoms clear up. If used for many weeks or months without a break, they can cause side effects. These include loss of skin color, thinning skin, and skin showing streaks or lines.
Creams or ointments with a calcineurin inhibitor such as tacrolimus (Protopic) or pimecrolimus (Elidel) may be effective. Another benefit is that they have fewer side effects than corticosteroids do. But they are not first-choice treatments because the Food and Drug Administration has concerns about a possible association with cancer. In addition, tacrolimus and pimecrolimus cost more than mild corticosteroid medications.
- Antifungal medication you take as a pill. If your condition isn't improving with other treatments or is severe, your health care provider may prescribe an antifungal medication in pill form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
ErrorEmail field is required
ErrorInclude a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Lifestyle and home remedies
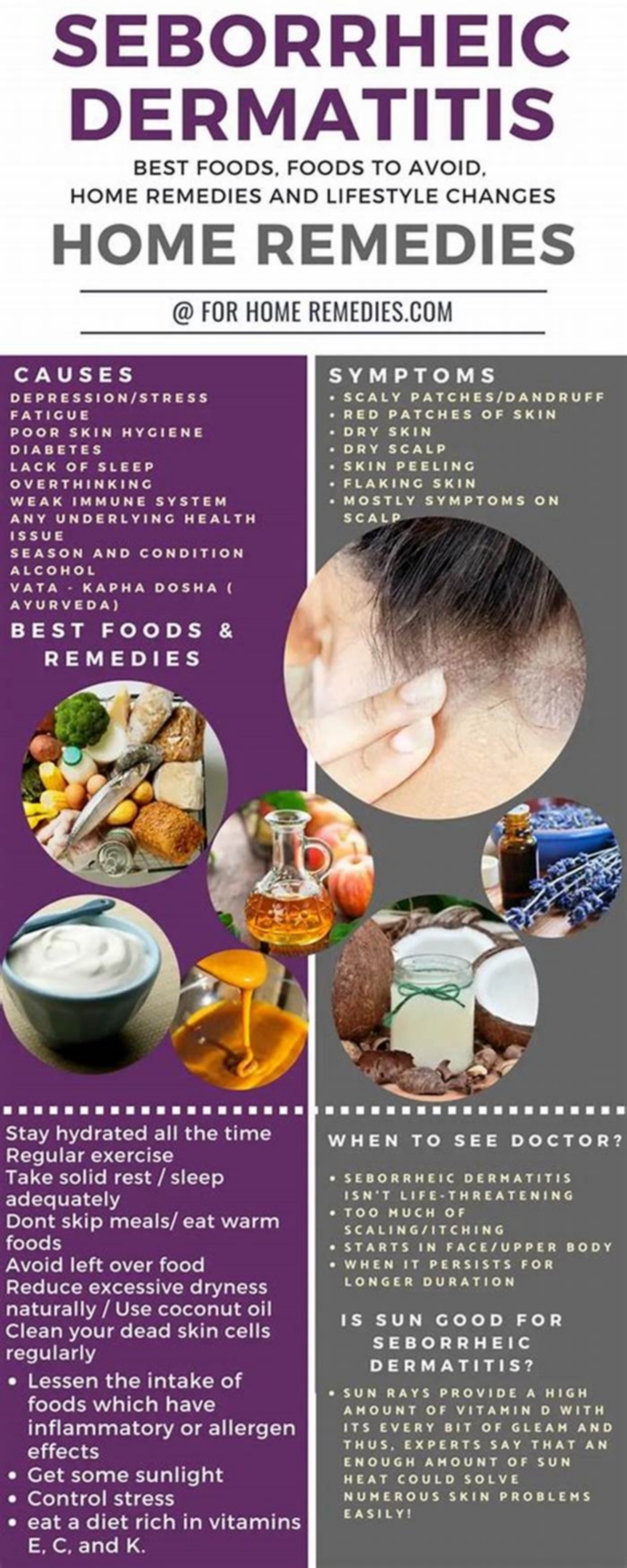
You may be able to control seborrheic dermatitis with lifestyle changes and home remedies. Many of these are sold in nonprescription forms. You may need to try different products or a combination of products before your condition improves.
The best approach for you depends on your skin type, hair-grooming practices and your symptoms. But even if your condition clears up, it's likely to come back at some point. Watch for the symptoms and resume treating the condition when it recurs. Or use nonprescription antidandruff products in your self-care routine to prevent flare-ups.
Wash your scalp regularly
If regular shampoo doesn't help with dandruff, try nonprescription dandruff shampoos. They are classified according to the active ingredient they contain:
- Pyrithione zinc (DermaZinc, Head & Shoulders, others), also sold as bar soap
- Selenium sulfide (Head & Shoulders, Selsun Blue, others)
- Ketoconazole 1% (Nizoral A-D)
- Tar (Denorex Extra Strength, DHS Tar, others)
- Salicylic acid (Denorex, DHS Sal, others)
How often you shampoo or apply other antifungal products will depend on your hair-grooming practices and symptoms. Medicated shampoos can be used once a day or 2 to 3 times a week for several weeks. After your symptoms clear up, use a medicated shampoo just once a week or once every two weeks. This will help prevent a relapse. Shampoo that contains tar or selenium sulfide can discolor light-colored hair.
Sometimes a shampoo that has helped loses its effectiveness over time. If that's the case, try alternating between two or more types. Be sure to leave your shampoo on for the full recommended time this allows its ingredients to work. Then rinse. These shampoos may be rubbed gently on the face, ears and chest and rinsed off well.
Other home remedies
The following nonprescription treatments and self-care tips may help you control seborrheic dermatitis:
- Soften and remove scales from your hair. Apply mineral oil, peanut oil or olive oil to your scalp. Leave it in for 1 to 3 hours. Then comb or brush your hair and wash it.
- Wash your skin regularly. Use warm, not hot, water and a gentle soap or nonsoap cleanser. Rinse thoroughly. Pat dry and apply a moisturizer while your skin is still damp.
- Apply a medicated cream. First try a mild corticosteroid cream, foam, ointment or oil (Scalpicin Scalp Itch) on affected areas, keeping it away from the eyes. If that doesn't work, try the antifungal cream ketoconazole.
- Don't use styling products. Stop using hair sprays, gels and other styling products while you're treating the condition.
- Don't use skin and hair products that contain alcohol. These can cause the disease to flare up.
- If you have a beard or mustache, shampoo facial hair regularly. Seborrheic dermatitis can be worse under mustaches and beards. Shampoo with 1% ketoconazole daily until your symptoms improve. Then switch to shampooing once a week or once every two weeks. Or shaving might ease your symptoms.
- Gently clean your eyelids. If your eyelids are inflamed or scaly, wash them each night. Use a few drops of baby shampoo mixed with two capfuls of warm water. Wipe away scales with a cotton swab. Warm, damp cloths pressed to your eyelids also may help.
- Gently wash your baby's scalp. If your infant has mild cradle cap, wash the scalp with a mild baby shampoo once a day. Gently loosen the scales with a cloth or an infant hairbrush before rinsing out the shampoo. If scaling persists, first apply mineral oil or olive oil to the scalp for an hour or two. Cradle cap usually disappears in a few weeks or months.
Alternative medicine
Many alternative therapies, including those listed below, have helped some people manage their seborrheic dermatitis. But evidence for their effectiveness isn't proved. It's always a good idea to check with your health care provider before adding any alternative medicines to your self-care routine.
- Tea tree oil. A shampoo with 5% tea tree oil may be used on the affected area. Some studies suggest that tea tree oil can trigger an allergic reaction.
- Aloe. Apply aloe vera gel to the affected area. Aloe is an ingredient in many products, or you can use it directly from the leaf of an aloe plant.
If you're considering dietary supplements or other alternative therapies, talk with your health care provider about their pros and cons.
Preparing for your appointment
You'll probably first visit your primary care provider. Or you may see a doctor who specializes in the diagnosis and treatment of skin conditions (dermatologist).
Here's some information to help you get ready for your appointment.
What you can do
Before your appointment, list your answers to the following questions:
- What are your symptoms, and when did they start?
- Does anything seem to trigger your symptoms?
- What medications are you taking, including those you take by mouth as well as creams or ointments?
- What treatments have you tried so far? Has anything helped?
What to expect from your doctor
Your health care provider is likely to ask you a few questions. Being ready to answer them may free up time to go over any points you want to spend more time on. Your health care provider might ask:
- What are your symptoms, and when did you first notice them?
- Is this the first time you've had these symptoms, or have you had them before?
- How severe are your symptoms? Are they about the same all the time, getting worse, or sometimes better and sometimes worse?
- Do your symptoms affect your quality of life, including your ability to sleep?
- Have you tried any at-home treatments, such as creams, gels or shampoos?
- How often do you use these treatments?
- Does anything seem to help?
- Does anything seem to make your symptoms worse?
- What medications, vitamins or supplements are you taking?
- Have you been under stress lately or experienced major life changes?
What you can do in the meantime
A nonprescription antifungal cream or anti-itch cream can be helpful. If your scalp is affected, a nonprescription antifungal shampoo, foam or other product may ease your symptoms. Try not to scratch or pick at the affected area. This increases your risk of infection.
Sept. 27, 2022
Seborrheic Dermatitis: A Dermatologist Talks Treatment
What is seborrheic dermatitis?
 Seborrheic dermatitis is a common skin condition that affects the areas of the body that have a high density of oil-producing (sebaceous) glands.
Seborrheic dermatitis is a common skin condition that affects the areas of the body that have a high density of oil-producing (sebaceous) glands.
It affects 1 to 5 percent of the general population, and often has a chronic, relapsing course.
The exact cause of seborrheic dermatitis is not completely clear, although genetic and hormonal influences have been shown to play a role in this condition. Furthermore, certain fungal microorganisms that live naturally on the skin, belonging to the genus Malassezia, can also contribute to seborrheic dermatitis.
Patients of any age can develop seborrheic dermatitis, including infants (in which it is known as cradle cap), teenagers, and adults.
Flares of seborrheic dermatitis have been associated with many factors, such as stress, hormonal changes, or illness. Skin irritants such as certain detergents, solvents, chemicals, and soaps may also worsen seborrheic dermatitis. In general, seborrheic dermatitis is slightly more common in men than in women. Patients with certain diseases that affect the immune system (such as HIV/AIDS) and the nervous system, such as Parkinsons disease, are also at increased risk of developing seborrheic dermatitis.
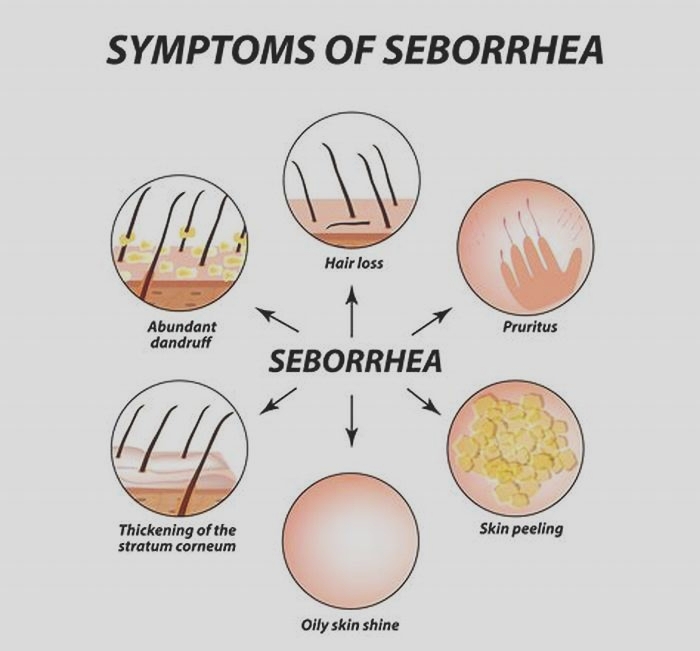
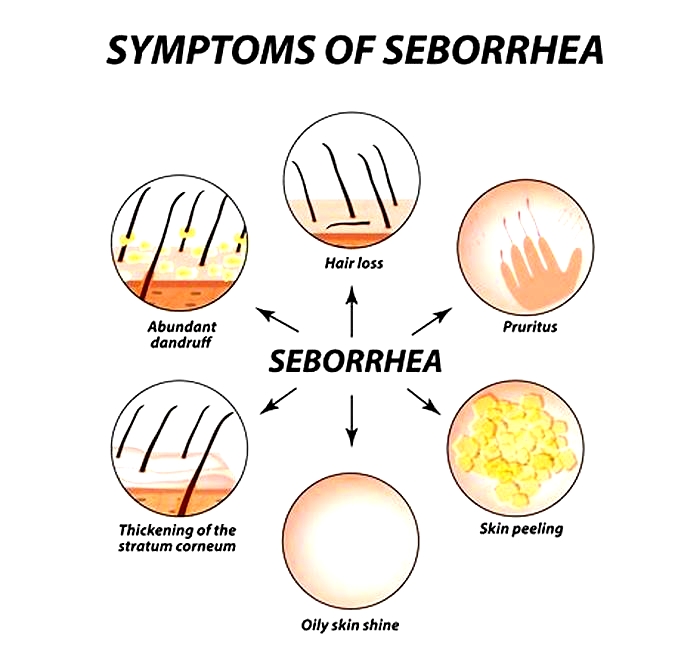
Seborrheic dermatitis mainly affects the scalp, where it may range from dry flakes (dandruff) to yellow, greasy scales with reddened underlying skin. Patients can also develop seborrheic dermatitis on other oily areas of their body, such as the face, upper chest and back. Seborrheic dermatitis is not harmful to a patients health, nor is it contagious, and fortunately complications are rare. It can, however, have a profound impact on a patients quality of life and emotional well-being.
How can you identify it?

Example of seborrheic dermatitis on the face. Photo courtesy of Skinsight.com, Logical Images, Inc.
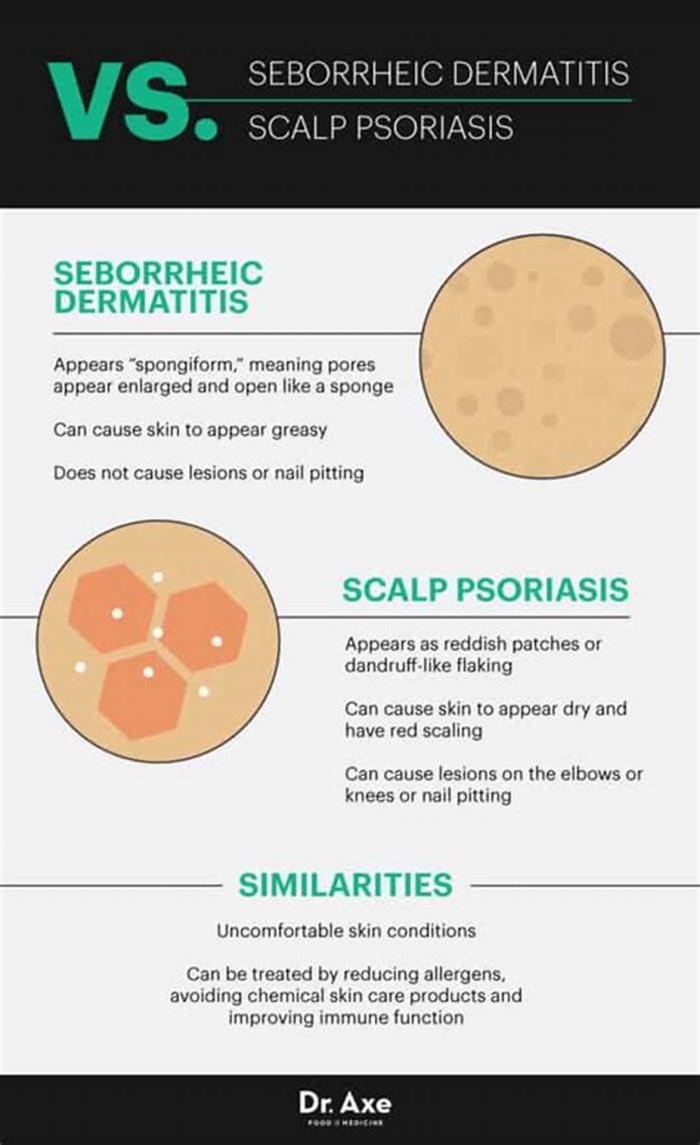
Seborrheic dermatitis can often resemble other skin conditions. The typical symptoms that patients with seborrheic dermatitis experience include redness, flaking, scaly patches, and sometimes itching of the affected skin. Like eczema and psoriasis, two other common skin diseases, seborrheic dermatitis produces inflammation of the skin.
Seborrheic dermatitis can look like and/or overlap with other skin conditions. If you are experiencing symptoms, it is important to see a dermatologist to get the correct diagnosis and treatment. There is no specific test for diagnosing seborrheic dermatitis. Your dermatologist will ask about your medical history and also perform a physical examination of your skin. Usually, these measures alone will be sufficient to make the diagnosis.
In certain cases, a scraping of skin under a drop of potassium hydroxide is examined under a microscope to exclude a fungal infection. Similarly, a skin biopsy (a procedure in which a small sample of skin is removed) may be required in rare cases to confirm the diagnosis or rule out other conditions that mimic seborrheic dermatitis.
How is seborrheic dermatitis different from atopic dermatitis?

Example of seborrheic dermatitis on the chest. Photo courtesy of Skinsight.com, Logical Images, Inc.
Atopic dermatitis and seborrheic dermatitis are both forms of eczema, a general term that describes inflammatory skin conditions that produce significant redness and itching. Not uncommonly, a single person can be diagnosed with both seborrheic dermatitis and atopic dermatitis. Atopic dermatitis nearly always produces itchy, red skin but seborrheic dermatitis is not always itchy. The areas of affected skin can also differ between both of these conditions. Distinct from seborrheic dermatitis, atopic dermatitis most often affects the face, hands, feet, inside of the elbows and behind the knees.
Additionally, Malassezia organisms are known to contribute to seborrheic dermatitis. As a result, the treatment approaches to atopic dermatitis and seborrheic dermatitis are different.
Topical medications such as steroids, pimecrolimus, and tacrolimus are traditionally used to help relieve symptoms of atopic dermatitis. But for seborrheic dermatitis, the treatments instead target fungi that like oil glands, like Malassezia.
Nonetheless, distinguishing between seborrheic dermatitis and atopic dermatitis can pose a challenge even for healthcare professionals, and it is therefore important to see a physician should you develop concerns about your skin.
How is seborrheic dermatitis treated?
The symptoms of seborrheic dermatitis can be effectively controlled, and currently a variety of medicated treatments are available both over the counter and by prescription. A combination of self-care measures and drug therapy is often required to optimally treat seborrheic dermatitis.
For adults, long-term maintenance may be necessary to control the symptoms of seborrheic dermatitis. Dandruff, which represents mild seborrheic dermatitis of the scalp, may be treated with over-the-counter anti-dandruff shampoos. These contain one of several available active ingredients: selenium sulfide, tar, zinc pyrithione, and ketoconazole. These have all been shown to be equally effective after four weeks of consistent use.
Antifungal solutions containing ketoconazole, such as the shampoo Nizoral, are considered mainstays of treatment because they kill fungi such as Malassezia. For best results, shampoos should be left in place for five to ten minutes before rinsing, and then rinsed out completely. Initially, medicated shampoos may be used every day, and then as symptoms improve, they can be tapered to every other day. If one shampoo does not improve symptoms after four to six weeks, then a different shampoo may be tried.
For seborrheic dermatitis affecting areas other than the scalp, topical steroids such as hydrocortisone can also alleviate the redness and itching. These may be applied once or twice daily for up to two weeks. Very rarely, a systemic medication (often in the form of a pill), such as an antifungal medication or steroid, may be required to control symptoms if they are severe.
Fortunately, although there is no permanent cure yet, seborrheic dermatitis often improves with an excellent response once treatment is started.
Ultimately, however, it is important to note that if symptoms fail to improve with therapy or worsen, then you should make an appointment with a health care provider to have your symptoms evaluated further.
Conclusion
In conclusion, seborrheic dermatitis is a condition that can be readily managed with a balance of self-care and medicated treatments. Patients experience improvement and flares intermittently throughout their disease course, which tends to be chronic.
Factors such as hormones, genes, exposures to chemicals, and stress can all potentially trigger flares of seborrheic dermatitis.
For overall health, it is also important to consult with your physician should you notice any changes in your skin, such as symptoms suggestive of seborrheic dermatitis.
 Monica Enamandram, M.D. is a resident physician at Memorial Sloan-Kettering Cancer Center. She earned her MD degree at Harvard Medical School, and will continue her residency training in Dermatology at Stanford University Hospitals. She is interested in patient education and clinical research in dermatology, and is excited to develop successful preventive measures and treatment regimens for eczema.
Monica Enamandram, M.D. is a resident physician at Memorial Sloan-Kettering Cancer Center. She earned her MD degree at Harvard Medical School, and will continue her residency training in Dermatology at Stanford University Hospitals. She is interested in patient education and clinical research in dermatology, and is excited to develop successful preventive measures and treatment regimens for eczema.