Is seborrhea a bacteria

9 Seborrhea Dog Shampoos: A Comprehensive Review
Seborrhea in dogs can be a challenging condition, but the right shampoo can make a world of difference. In this guide, we delve deep into the world of seborrhea dog shampoos, offering you a detailed analysis of 9 top products.
Understanding Seborrhea in Dogs
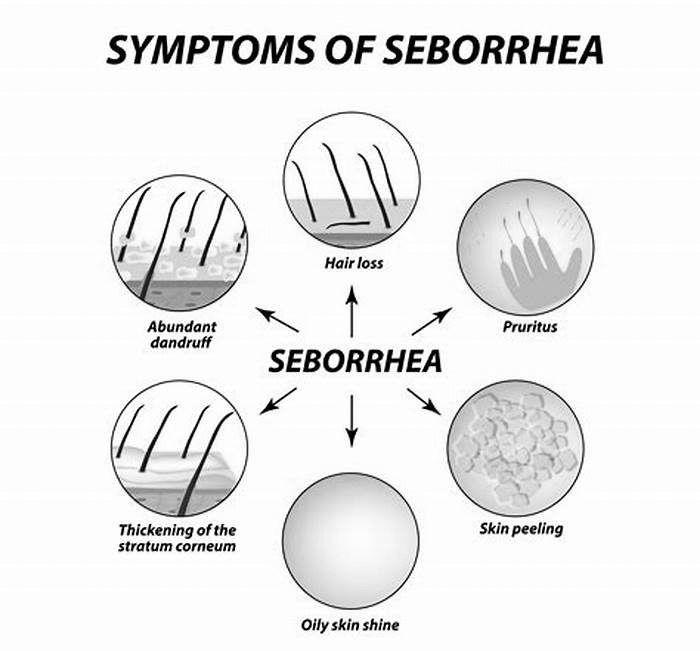
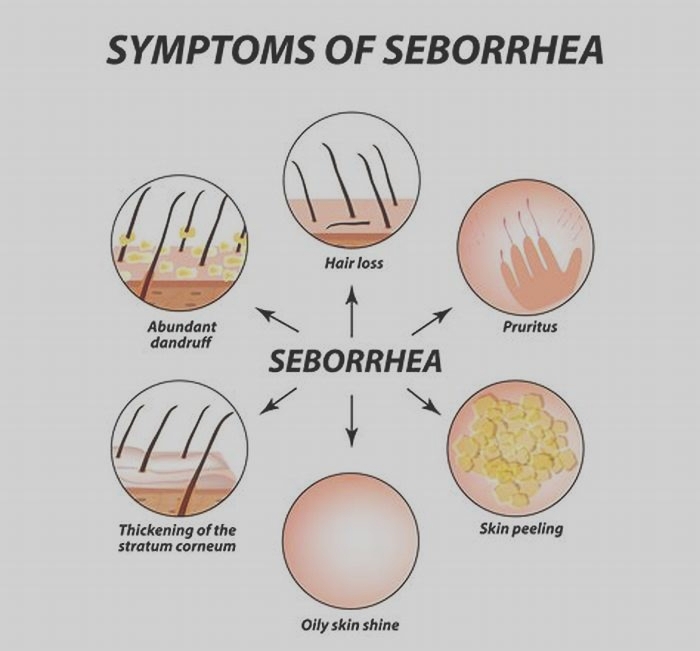
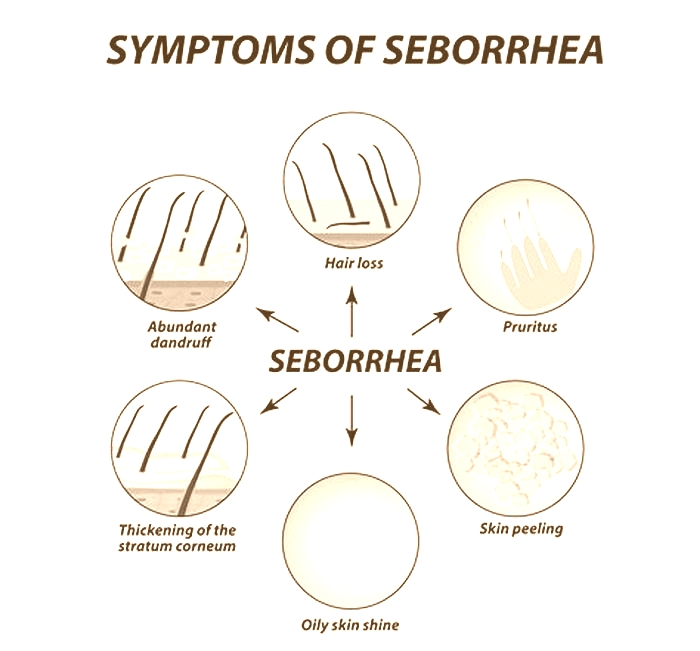
Before we jump into the shampoos, lets quickly understand what seborrhea is. Its a skin condition in dogs that results in excessive oil production and flaky dandruff. This can lead to itching, discomfort, and even secondary infections.
Top 9 Seborrhea Dog Shampoos: A Detailed Look
Weve analyzed various shampoos based on their ingredients, effectiveness, and suitability for different severities of seborrhea. Heres a comprehensive table chart for a quick overview:
| Shampoo Name | Key Ingredients | Action | Pros | Cons | Best For |
|---|---|---|---|---|---|
| Epi-Pet Medicated | Chlorhexidine, Ketoconazole, Salicylic Acid | Combats infections, yeast overgrowth | Powerful ingredients, long-lasting | Can be harsh, vet consultation needed | Severe Cases |
| Natures Miracle | Oatmeal, Aloe Vera, Coconut Oil | Soothes, moisturizes | Gentle, natural, affordable | Less effective for severe cases | Mild Seborrhea |
| Wahl Oatmeal Itch Relief | Oatmeal, Colloidal Oatmeal, Vitamin E | Reduces inflammation, calms itchiness | Affordable, gentle | Less potent for aggressive seborrhea | Mild to Moderate Cases |
| Douxo Chlorhexidine & Miconazole | Chlorhexidine, Miconazole, Piroctone Olamine | Tackles bacterial and fungal infections | Prescription-quality, tackles multiple issues | Can be harsh, vet consultation needed | Chronic Seborrhea |
| Pet MD Bio Spot Active Care | Chlorhexidine, Miconazole, Pyrethrins | Treats infections, addresses parasites | Broad-spectrum, long-lasting | Can be harsh, vet consultation needed | Heavily Affected Dogs |
| Earthbath Oatmeal & Aloe | Oatmeal, Aloe Vera, Coconut Oil | Gently cleanses, soothes | Natural ingredients, gentle | Not for severe cases | Mild Seborrhea, Sensitive Dogs |
| Veterinary Formula Clinical Care | Chlorhexidine, Aloe Vera, Hydrocortisone | Combats bacteria, soothes inflammation | Clinically proven, multiple concerns | Can be harsh, vet consultation needed | Inflamed Seborrhea |
| Zymox Otic & Seborrheic | Chlorhexidine, Miconazole, Enzymes | Reduces odor, combats infections | Effective for greasy coats, long-lasting | Can be harsh, vet consultation needed | Chronic, Greasy Seborrhea |
| Pawsome Organics | Oatmeal, Aloe Vera, Jojoba Oil | Cleanses gently, soothes skin | Natural ingredients, gentle | Less effective for severe cases | Mild Seborrhea, Sensitive Dogs |
1. Epi-Pet Medicated Chlorhexidine Shampoo
Best for Severe Cases: This shampoo is a powerhouse against severe seborrhea. Its combination of antibacterial and antifungal ingredients makes it ideal for dogs suffering from secondary infections due to seborrhea.
2. Natures Miracle Hypoallergenic Oatmeal & Aloe Shampoo
Best for Mild Seborrhea: A perfect choice for dogs with sensitive skin. Its natural ingredients offer a soothing and moisturizing effect, making bath time a calming experience.
3. Wahl Oatmeal Itch Relief Pet Shampoo
Best for Regular Maintenance: Ideal for dogs with mild to moderate seborrhea. Its gentle enough for frequent use, helping maintain a healthy coat without being too harsh.
4. Douxo Chlorhexidine & Miconazole Shampoo
Best for Chronic Seborrhea: This shampoo is a go-to for long-term management of chronic seborrhea. It effectively tackles both bacterial and fungal issues, providing relief for greasy and malodorous coats.
5. Pet MD Bio Spot Active Care Medicated Dog Shampoo
Best for Dogs with Parasite Issues: Not only does it address seborrhea, but its also effective against flea and mite infestations, making it a comprehensive solution for dogs with multiple skin issues.
6. Earthbath Oatmeal & Aloe Shampoo
Best for Sensitive Dogs: Its natural formulation is perfect for dogs with sensitive skin. It gently cleanses while providing the necessary relief from irritation and dryness.
7. Veterinary Formula Clinical Care Chlorhexidine Shampoo
Best for Inflamed Seborrhea: This shampoo is particularly effective for dogs with inflamed skin due to seborrhea. It not only combats bacteria but also provides much-needed relief from itchiness and inflammation.
8. Zymox Otic & Seborrheic Pet Shampoo
Best for Greasy Coats: If your dog suffers from a greasy coat due to seborrhea, this shampoo can be a game-changer. It effectively reduces odor and manages the greasiness associated with the condition.
9. Pawsome Organics Oatmeal & Aloe Dog Shampoo
Best for Everyday Use: For dogs with mild seborrhea or those who need a gentle shampoo for regular use, this is an excellent choice. Its soothing ingredients ensure a comfortable bath time.
Key Takeaways
Choose Based on Severity: The severity of your dogs seborrhea should guide your choice of shampoo.
Natural Ingredients for Mild Cases: For mild seborrhea, shampoos with natural ingredients like oatmeal and aloe vera are ideal.
Consult Your Vet: For severe cases, consider shampoos with stronger ingredients, but always consult your vet first.
Regular Bathing Routine: Establishing a regular bathing routine with the right shampoo can significantly improve your dogs skin condition.
Conclusion
Managing seborrhea in dogs requires a thoughtful approach, and choosing the right shampoo is a crucial part of this process. By understanding the specific needs of your dog and the benefits of each shampoo, you can make an informed decision that will help alleviate your dogs discomfort and improve their skin health. Remember, a happy dog means a happy life!
FAQs on Seborrhea Dog Shampoos
How Often Should I Bathe My Dog with Seborrhea Shampoo?
The frequency of bathing depends on the severity of seborrhea and the type of shampoo used. For mild seborrhea, once a week with a gentle shampoo like Pawsome Organics or Earthbath Oatmeal & Aloe may suffice. In more severe cases, your vet might recommend bathing two to three times a week with a medicated shampoo like Epi-Pet Medicated or Douxo Chlorhexidine & Miconazole. Its crucial to follow your vets advice to avoid over-drying your dogs skin.
Can Human Dandruff Shampoos Be Used on Dogs?
No, human dandruff shampoos should not be used on dogs. The pH balance of dog skin is different from humans, and human shampoos can disrupt the skins natural barrier, leading to more severe skin issues. Always use a shampoo formulated specifically for dogs.
Are There Any Natural Remedies for Seborrhea in Dogs?
While natural remedies cant replace veterinary care, they can complement it. Oatmeal baths (using colloidal oatmeal) can soothe irritated skin. Omega-3 fatty acid supplements may also help improve skin health. However, its important to consult with your vet before trying any natural remedies.
How Can I Tell if the Shampoo is Working?
You should see a reduction in flakiness, oiliness, and itchiness of your dogs skin. Improvement usually becomes noticeable after a few baths. If your dogs skin condition doesnt improve or worsens, consult your vet. They might recommend a different shampoo or investigate other underlying causes.
Can Seborrhea Shampoos Help with Dog Odor?
Yes, many seborrhea shampoos, especially those containing chlorhexidine and miconazole like Zymox Otic & Seborrheic Pet Shampoo, are effective in reducing the unpleasant odor associated with seborrhea. These shampoos target the yeast and bacteria that often contribute to the smell.
Is It Necessary to Use a Conditioner After a Seborrhea Shampoo?
Using a conditioner can be beneficial, especially if the shampoo is medicated and potentially drying. A conditioner formulated for dogs can help restore moisture and protect the skins barrier. Look for products with natural moisturizing ingredients like aloe vera or coconut oil.
What Precautions Should I Take When Using Medicated Shampoos?
When using medicated shampoos:
- Avoid contact with your dogs eyes and ears.
- Wear gloves to protect your skin.
- Rinse thoroughly to prevent residue buildup.
- Monitor your dog for any adverse reactions, such as increased itching or redness.
Can Diet Affect Seborrhea in Dogs?
Yes, diet plays a significant role in skin health. A balanced diet rich in essential fatty acids, particularly omega-3 and omega-6, can help improve skin conditions. Some dogs may benefit from a hypoallergenic diet if food allergies contribute to their skin issues. Consult with a veterinarian for dietary recommendations tailored to your dogs specific needs.
Should I Brush My Dogs Coat When Dealing with Seborrhea?
Regular brushing helps distribute natural oils, remove loose fur, and reduce skin flakiness. Use a soft-bristle brush or a suitable grooming tool for your dogs coat type. Brushing also enhances the effectiveness of shampoos by removing debris and allowing better skin contact.
Can Seborrhea Lead to Other Health Issues in Dogs?
If left untreated, seborrhea can lead to more serious conditions like secondary bacterial or fungal infections. Chronic skin irritation and scratching can also cause hair loss and thickened skin. Regular veterinary check-ups and proper management are essential to prevent complications.
How Does Seborrhea Affect Different Dog Breeds?
Seborrhea can manifest differently across various dog breeds. Breeds with dense or oily coats, like Cocker Spaniels or Basset Hounds, might be more prone to oily seborrhea, characterized by a greasy coat and strong odor. Conversely, breeds with thinner coats may exhibit dry seborrhea, resulting in excessive flakiness and dandruff. Understanding breed-specific predispositions can guide the choice of shampoo and treatment approach.
Is There a Seasonal Variation in Seborrhea Symptoms in Dogs?
Yes, seborrhea symptoms in dogs can fluctuate with seasons. In colder months, indoor heating can dry out a dogs skin, potentially exacerbating dry seborrhea. During warmer, more humid seasons, dogs might experience an increase in oily seborrhea. Adjusting the bathing routine and shampoo type according to seasonal changes can help manage these variations effectively.
Can Stress Exacerbate Seborrhea in Dogs?
Stress can indeed impact a dogs skin health. Dogs experiencing stress or anxiety may show an increase in skin problems, including the symptoms of seborrhea. Stress-induced hormonal changes can alter skin oil production and immunity, making effective stress management an integral part of treating seborrhea.
What Role Does Grooming Play in Managing Seborrhea?
Regular grooming goes beyond mere aesthetics; its vital for managing seborrhea. Grooming helps remove scale buildup, distribute natural skin oils, and increase the effectiveness of medicated shampoos. For breeds with long or dense coats, professional grooming might be necessary to ensure thorough cleaning and care.
How Long Does It Typically Take to See Improvement in Seborrhea Symptoms?
The time frame for improvement varies depending on the severity of the condition and the treatment approach. Some dogs may show noticeable improvement within a few weeks of consistent shampoo therapy, while others with more severe conditions might take longer. Continuous evaluation and possible adjustments in treatment are essential for optimal results.
Are There Any Lifestyle Changes That Can Help Manage Seborrhea in Dogs?
Lifestyle changes can significantly impact the management of seborrhea. Ensuring your dog has a balanced diet, regular exercise, and a stress-free environment can improve overall skin health. Additionally, maintaining a consistent grooming and bathing schedule is crucial in managing seborrhea symptoms.
How Can I Safely Transition to a New Seborrhea Shampoo?
When transitioning to a new seborrhea shampoo, its advisable to do so gradually. Start by mixing the new shampoo with the old one in small amounts, gradually increasing the proportion. This method helps your dogs skin adjust to the new formulation, reducing the risk of adverse reactions.
Can Environmental Allergens Worsen Seborrhea in Dogs?
Environmental allergens like pollen, dust, or mold can exacerbate seborrhea symptoms. Dogs with a predisposition to allergies may experience more severe skin reactions during high-allergen seasons. Keeping the home environment clean and using air purifiers can help reduce exposure to these allergens.
What Are the Signs That a Seborrhea Shampoo Isnt Suitable for My Dog?
If a seborrhea shampoo is not suitable, you might notice signs like increased skin redness, persistent itching, worsening of skin flakiness, or new skin lesions. If any of these symptoms occur, discontinue the shampoo and consult your veterinarian for an alternative treatment plan.
How Important Is the pH Balance of a Seborrhea Shampoo?
The pH balance of a seborrhea shampoo is crucial. Dogs have a different skin pH than humans, usually more neutral. Using a shampoo with an inappropriate pH can disrupt the skins natural barrier, leading to increased irritation and exacerbation of seborrhea symptoms. Always choose a shampoo specifically formulated for canine skin pH.
HELP US PUT FOOD ON THE TABLE
Bookshelf
Continuing Education Activity
Seborrheic dermatitis is a common papulosquamous skin disease that is most prevalent in infancy and middle age, and it usually presents differently in these two age groups. This activity will help to identify the different presentations of seborrheic dermatitis and illustrate how each may influence management decision making that leads to improved treatment outcomes.
Objectives:
Describe the burden of seborrheic dermatitis from an epidemiological, clinical, and economic perspective and be aware of its potential to impair quality of life.
Identify the hypotheses concerned with understanding the diverse pathophysiological mechanisms underlying the development of seborrheic dermatitis.
Explain the reasons for the relevant differential diagnoses for seborrheic dermatitis in the younger and older cohorts.
Outline an evidence-based formulary for the treatment of seborrheic dermatitis that includes conservative measures, over-the-counter products, and prescription treatments that are age-appropriate and likely to improve compliance, along with facilitating the variation of treatment at home. Good communication, patient education, and involvement of the dermatologist and pharmacist in the identification of suitable treatments are all important in this regard.
Introduction
Seborrheic dermatitis (SD) is a common inflammatory skin disease presenting with a papulosquamous morphology in areas rich in sebaceous glands, particularly the scalp, face, and body folds. The infantile (ISD) and adult (ASD) variants reflect the conditions bimodal occurrence.
Infants are not usually troubled by seborrheic dermatitis, but it may cause significant parental anxiety, often appearing as firm, greasy scales on the crown and frontal regions of the scalp. It occurs in the first three months of life and is mild,self-limiting, and resolving spontaneously in most cases by the first year of life.ASD, on the other hand, is characterized by a relapsingand remitting pattern of disease and isranked third behind atopicand contact dermatitis for its potential to impair the quality of life.[1]
Etiology
There are multiple factors associated with the development ofseborrheic dermatitis, and their disparate nature has led to many proposals about its cause and pathogenesis, but the onset of SD appears linked to the interplay of normal microscopic skin flora (especially Malassezia spp.), the composition of lipids on the skin surface and individual susceptibility. Neither the level of sebum produced nor the amount of yeast appears to be significant factors.[2]
Epidemiology
The worldwide prevalence of seborrheic dermatitis is around 5%, but the prevalence of its non-inflammatory variant, dandruff, is probably closer to 50%. SD affects all ethnic groups in all regions globally.[3]The prevalence of SD is bimodal with a peak in the first three months of life and then from adrenarche to a second peak after the fourth decade. In Australian preschool children, the prevalence of SD was approximately 72% at three months then fell rapidly with an overall incidence of 10%. Furthermore, analysis of the Rotterdam Study data found that 14% of middle-aged and elderly adults had SD.[4]In HIV-AIDS, however, 35% with early HIV infection have SD, and the prevalence reaches 85% in patients with AIDS.[5]
Risk factors for the development of seborrheic dermatitis include:
Age
Male sex
Increased sebaceous gland activity
Immunodeficiency, including
[6]:
Lymphoma
Renal transplantation
HIV-AIDS
Neurologicaland psychiatric disease, including
[7]:
Parkinson disease
Stroke
Alzheimer dementia
Major depression
Autonomic dysfunction
Exposure to drug treatment, including:
Dopamine antagonists
Immunosuppressants
Psoralen/PUVA
Lithium
Low ambient humidity and/or low ambient temperature
Pathophysiology
Proposed mechanisms for thepathogenesis of seborrheic dermatitisinclude[8][9][10]:
Disruption of the skins microbiota
An impaired immune reaction to Malassezia spp. associated with a diminished T-cell response and activation of complement
The increased presence of unsaturated fatty acids on the skin surface
Disruption of cutaneous neurotransmitters
Abnormal shedding of keratinocytes
Epidermal barrier disturbances associated with genetic factors
The role of Malassezia spp. also includes the degradation of sebumand consumption of saturated fatty acids, disrupting the lipid balance on the skin surface.Further evidence for the involvement of Malassezia spp. includes their isolation from SD lesions andthe significant resolution of SD with antifungal treatment.
However, there is insufficient evidence to link ISD with the development of ASD.
Histopathology
The dermatopathology of seborrheic dermatitis is non-specific, but the surface and infundibular epidermis usually show a superficial perivascular infiltrate of lymphocytes, acanthosis, focal spongiosis, and focal parakeratosis.[11][12]Shoulder parakeratosis refers to scale-crust accumulation around the infundibular ostia. Malassezia may be present in the stratum corneum.
Histological progression from acute to chronic SD characteristically demonstrates a transition from spongiosis to psoriasiform hyperplasia and the development of a lichenoid lymphocytic infiltrate.Severe SD is often associated with keratinocyte necrosis, focal interface destruction, and leukocytoclasis.
History and Physical
The distribution of lesions is the most important clinical feature of seborrheic dermatitis, with lesions occurring in areas where the skin is rich in sebaceous glands, especially on the scalp and face. ISD is generally asymptomatic, but atopic dermatitis frequently coexists. On the other hand, pruritus is common in ASD, especially with scalp lesions, and patients regularly report burning, but there is usually no history of atopic dermatitis.Seborrheic dermatitis characteristically demonstrates folliculocentric salmon-colored papules and plaques with a fine white scale, and a yellowish crust often described as a greasy scale-crust. It may present in one or more locations, with less scaling on flexural surfaces, and with lesions whose margins tend to be poorly defined.
The mildest form of SD is a non-inflammatory variant commonly referred to as pityriasis capitis or sicca.[12]It affects the scalpand beard region and is associated with the shedding of small light-colored flakes of skin, often seen on a background of dark clothing as dandruff. Sudden onset of severe SD should be a red flag for the presence of HIV-AIDS, with early recognition and diagnosis of HIV-AIDS significantly improving long-term outcomes. Common clinical presentations include reddening of the face, scaling, and dandruff. On darker skin, there may be persistent dyschromia with variable hyper/hypo-pigmentation. Other conditions associated with Malassezia spp may be present, including pityriasis versicolorand (Pityrosporum/Malassezia) folliculitis in adults and neonatal cephalic pustulosis.[13]Lesions on the anterior chest tend to have a psoriasiform morphology but frequently have a petaloid appearance, with such annular lesions commonly observed on the face in darker skin phenotypes. A pityriasiform variation (with a collarette scale mimicking pityriasis rosea) is rare.
Adult SD:
The face, scalp, and chest arethesites most commonly involved in ASD, witharound 88%, 70%, and 27% of cases developing lesions in these areas, respectively.[14]On the headand neck, seborrheic dermatitis is characteristically symmetrical and involves the central third of the face, including the malar region, the center of the forehead, the eyebrows (especially their medial aspects), the postauricular area, and the external ear canal. SD characteristically affects the nasolabial and alar folds, and blepharitis is a common finding with the involvement of the anterior (lash) line.
Psoriasis requires differentiating from seborrheic dermatitis in adults. It is characterized by indurated red papulesand plaques that have a sharply defined margin and a loose, silvery lamella scale. The nails may show psoriatic changes, and the Auspitz sign is positive. The existence of sebopsoriasis as a separate clinical entity has come into dispute.[7]
Infantile SD:
ISD usually appears in the second week of life and tends to last 4 to 6 months. It can present in the facial distribution of ASD, the diaper region, the skin creases of the neck, and the axillae. The rash is usually not itchy or painful, and the infants look content, but parents may be distressed. It is generally mildand self-limiting. A common presentationknown ascradle cap refers to as an adherent yellowish scale-crust that arises on the crown and front of the scalp, developing from a bran-like scale, serous ooze, and a greasy crust, to create a firm mass that may progress to involve the whole scalp.
Pityriasisamiantacea may be present in ISD. It represents a set of clinical findings that may occur in older infants or young children but is not specific to seborrheic dermatitis. Typically, there are thick, silvery or yellow scales enveloping scalp hairs and binding them in tufts and can also be present in scalp psoriasis, atopic dermatitis, and tinea capitis. Atopic dermatitis is important in the differential diagnosis of ISD. It tends to be pruriticand prone to weeping and typically occurs on the faceand limb flexures (elbow and knee) and spares the trunk. The child tends to be upset by the rash, and scratch marks are a common finding.
Evaluation
It is not necessary to routinely investigate seborrheic dermatitis, but HIV serology should be expedited in cases of severe SD, especially where the onset is sudden. Clinical features of Parkinson disease require recognition in elderly patients.The patients medications require a review.
The following tests may be helpful in the differential diagnosis
KOH examination of skin scrapings
Swab for microscopy, culture, and sensitivities
Histologyand direct immunofluorescence
HIV serology; VDRL
Serum zinc levels
ANA; ENA; ESR
Treatment / Management
The approach will vary according to the patients age and the distributionand severity of the condition. It is essential to discuss good general skincare practices, including the use of a soap-substitute and appropriate moisturizing.[15]Treatments should address the underlying disease process and any secondary features, especially the hyperkeratotic scale, Staphylococcal infection, and associated symptoms, particularly pruritus.A Danish expert group recommended that authorities adopt topical antifungals as first-line treatment and agreed that topical corticosteroidsand calcineurin inhibitors should only be used for significant symptoms and to manage moderate to severe flare-ups.[16]In ISD, removing the scale-crust in cradle cap and allaying parental anxiety are important considerations.[17]Sorbolene cream or lotion and a soft-bristled toothbrush can be used to soften and remove the cradle cap scales. On the other hand, it is crucial to relieve itch and discomfort in ASD.
A typical formulary should include antifungals, keratolytics, antipruritics, and anti-inflammatories (topical corticosteroidsand calcineurin inhibitors).Moreover, treatment rotation may be more effective and associated with fewer adverse reactions than persisting with monotherapy.For scalpand non-scalp SD treatment, evidence supports the use of topical 1%to 2% ketoconazole, 1% ciclopirox, 1% zinc pyrithione, and 1% hydrocortisone.[18]Intermittent use of a mild topical corticosteroidand imidazole antifungal combination is convenient and can be very effective, but a potent corticosteroid may be necessary for short term treatment of scalp ASD.Shampoos usually contain combinations of agents such as pine or coal tar (antipruritic/keratolytic), salicylic acid (keratolytic), sulfur (antimicrobial/keratolytic), and sulfacetamide (anti-inflammatory/antibacterial). The patient can apply these to the scalpand non-scalp regions and washed-off after 5to 10 minutes. Care should be taken when using topical salicylic acid, selenium, or zinc for the treatment of ISD, given the lack of safety and efficacy data to inform such treatment, but topical ketoconazole has been shown to be safe in infants with minimal systemic absorption detected.
Side effects associated with topical corticosteroids should be mitigated by intermittent use of site-appropriate potencies or steroid-sparing preparations such as topical 1% pimecrolimus. Another strategy is to employ the inherent anti-inflammatory effect of the topical antifungals, estimated to be equivalent to 1% hydrocortisone.[19]Oral treatment should be a consideration for generalized or refractory disease, and the standard of care utilizes the antifungaland anti-inflammatory properties of ketoconazole (monitor liver function; Black Box warning), itraconazole (check for CYP450 drug interactions; can worsen heart failure), and fluconazole (adjust the dose according to renal function). Itraconazole has the greatest anti-inflammatory effect, while oral terbinafine may be more effective than oral fluconazole in severe SD. Low-dose isotretinoin is non-inferior to topical standard of care but is commonly associated with significant mucocutaneous side effects.[20]
Itraconazole is safe and effective for controlling flares of SD and in preventing relapses.[19]It has also been shown to improve the quality of life in patients with moderate to severe SD.[21]However, given the absence of high-quality safety and efficacy data, a specialist team review is recommended before commencing oral treatment for ISD.In HIV-AIDS, antiretroviral treatment frequently improves SD, and SD may improve with L-dopa therapy in Parkinsons disease.[22]Future therapies for SD could target improving skin barrier function or restoring the skins surface lipid composition.
Typical Formulary May Include:
i. Topical Creams, Ointments, and Lotions
2% salicylic acid + 2% sulfur in sorbolene cream or emulsifying ointment
2% ketoconazole cream
1% clotrimazole + 1% hydrocortisone cream
10% sulfacetamide + 5% sulfur lotion
Betamethasone dipropionate 0.05% lotion
0.03% and 0.1% tacrolimusointment
ii. Shampoos
1% zinc pyrithione
1%to .5% selenium sulfide
2% ketoconazole
1% ciclopirox
5% coal tar + 2% salicylic acid
0.1%and 0.03% tacrolimus
iii. Oral Medication
Itraconazole
Fluconazole
Terbinafine
Differential Diagnosis
Important Considerations in the Differential Diagnosis for Adult SD
Scalp
Psoriasis - usually nonpruritic and tends to affect the occipital and frontal regions, whereas SD tends to affect the vertex and parietal regions
Eczema (contact) -due to the use of different shampoo and hair dye
Dariers disease - yellowish-brown clusters of rough dome-shaped papules in Seborrheic distribution; acanthosis
Face
Psoriasis - rarely occurs in isolation; pitted nails
Lupus erythematosus (LE) discoid LE is associated with skin atrophyand scarring alopecia
Rosacea look for erythemaand telangiectasia; it may cause Meibomianitis, along the posterior lid line
Acne vulgaris look for comedones, which are its hallmark
Staphylococcal blepharitis (anterior lash line)
Eczema (contact) - eyelids commonly involved (irritant - dry, scaly; or allergic - swollen, vesicular)
Dariers disease- Nail changes
Trunk
Psoriasis - sharply-defined red plaques with a loose, silvery lamella scale
Pityriasis rosea - herald spot; collarette scale; Christmas tree distribution
Pityriasis versicolor - not symmetrical; hypo/hyperpigmentation
Subacute lupus erythematosus - photosensitive distribution
Eczema (nummular) - intense pruritus
Tinea corporis - raised leading edgesand central clearing; uncommon in infants
Erythema annulare centrifugum - recurrent polycyclic lesions that slowly expand and disappear
Darier disease - Greasy wart-like papules and plaques
Grover disease (transient acantholytic dermatosis) - acanthosis
Drug reaction - drug history (neuroleptic; immunosuppressant; PUVA; lithium)
Parapsoriasis - elderly; very slow growing; resistant to treatment
Pemphigus foliaceus - fragile, painful blisters - Nikolsky sign is positive
Secondary syphilis - lesions on the palmsand soles; a history of chancre
Intertriginous Areas
Psoriasis (inverse) - sharply-defined border
Dermatitis (Contact) - itchy; vesicular
Tinea cruris - advancing border; very uncommon in infants
Erythrasma - coral-red fluorescence under Wood Lamp
Candidiasis - satellite lesions; obesity; a history of immunodeficiency
Hailey-Hailey disease (familial benign pemphigus) - acanthosis
Important Considerations in the Differential Diagnosis for ISD
Cradle Cap
Tinea capitis - (look for broken hairs or black dots); very uncommon in adults
Impetigo - yellow, honey-colored crusting
Diaper Region
Irritant contact dermatitis tends to spare the skin folds
Candidiasis either secondary or from colonization with fecal yeast; look for satellite lesions
Infantile psoriasis sharply-defined red plaques with silver scale
Histiocytosis X (Langerhans cell histiocytosis) tends to be confined to the skin folds with a purpuric rash on the body
Acrodermatitis enteropathica look for periorificial involvement and check zinc levels
Prognosis
ISD usually affects the scalp and is mildand self-limiting, whereas ASD presents a chronic pattern of skin disease characterized by relapsesand remissions. ASD is very controllable but not curable.
Complications
Seborrheic dermatitis usually takes a benign course, and serious complications are very rare. The intertriginous areasand eyelids are prone to secondary bacterial infections, especially during acute flares, and the diaper region is particularly prone to overgrowth with Candida spp.
Erythroderma has been reported in immunosuppressed neonates with generalized ISD, but it is more frequently a feature in adults with HIV-AIDS. However, research has not firmly established that SDcauses erythroderma per se, given its predilection for sebaceous-rich skin.[7][13]The most common problems associated with both ISD and ASD relate to misdiagnosis of the condition.[23]
Deterrence and Patient Education
Parental education isuseful in allaying anxiety associated with ISD, and well-informed adults can learn to be confident at managing their condition
For ASD, it requires emphasizing to the patient that there is no cure, but it can be well controlled and managed primarilyat home.
[16]Many of the treatments for SD are available without a prescription, over the counter at the pharmacy, or increasingly on supermarket shelves. Directing the patient to the selection of such products may save consultation time and associated costs.
Enhancing Healthcare Team Outcomes
SD is a difficult condition to manage in the adult, and its management is best by an interprofessional team.
Consider the impact of SD on psychosocial functioningand quality-of-life and remember that SD may accompany neurological or psychiatric disease.
[24]The dermatologistand pharmacist can help to promote the appropriate use of topical corticosteroids and employ steroid-sparing alternatives.
New evidence suggests diet may play a role in SD, with a high fruit intake associated with a 25% lower risk of SD, whereas a Western diet was associated with a 47% increased risk of SD.
[25]Atopic dermatitis and ISD frequently coexist, whereas psoriasis often occurs in adults with SD, but there is usually no history of atopic dermatitis
Review the diagnosis in recalcitrant cases of SD and consider immunodeficiency in sudden, severe cases
Topical antifungals have an anti-inflammatory effect which contributes significantly to their efficacy and is a convenient steroid-sparing strategy
Even though primary clinicians manage the condition, it is best to refer the complex patient to the dermatologist for guidance. Dermatology specialty-trained nurses can also help by counseling the patient, providing direction on medical management, and monitoring and charting treatment progress. A pharmacist should also be on the case, with assistance in selecting the most appropriate agents, verifying dosing, offering patient education, and performing medication reconciliation, informing the prescriber of any issues encountered. Close communication between interprofessional team members is vital to improving outcomes.
Infantile Seborrhoeic Dermatitis DermNet New Zealand
Seborrhoeic Dermatitis DermNet New Zealand
Seborrhoeic Keratoses DermNet New Zealand
Seborrheic Dermatitis Contributed by S bhimji, MD
References
- 1.
Sampogna F, Linder D, Piaserico S, Altomare G, Bortune M, Calzavara-Pinton P, Vedove CD, Girolomoni G, Peserico A, Sala R, Abeni D. Quality of life assessment of patients with scalp dermatitis using the Italian version of the Scalpdex.
Acta Derm Venereol. 2014 Jul;94(4):411-4.[
PubMed: 24287710]
- 2.
Zani MB, Soares RC, Arruda AC, de Arruda LH, Paulino LC. Ketoconazole does not decrease fungal amount in patients with seborrhoeic dermatitis.
Br J Dermatol. 2016 Aug;175(2):417-21.[
PubMed: 26920094]
- 3.
Palamaras I, Kyriakis KP, Stavrianeas NG. Seborrheic dermatitis: lifetime detection rates.
J Eur Acad Dermatol Venereol. 2012 Apr;26(4):524-6.[
PubMed: 21521374]
- 4.
Sanders MGH, Pardo LM, Franco OH, Ginger RS, Nijsten T. Prevalence and determinants of seborrhoeic dermatitis in a middle-aged and elderly population: the Rotterdam Study.
Br J Dermatol. 2018 Jan;178(1):148-153.[
PubMed: 28856679]
- 5.
Scognamiglio P, Chiaradia G, De Carli G, Giuliani M, Mastroianni CM, Aviani Barbacci S, Buonomini AR, Grisetti S, Sampaolesi A, Corpolongo A, Orchi N, Puro V, Ippolito G, Girardi E., SENDIH Study Group. The potential impact of routine testing of individuals with HIV indicator diseases in order to prevent late HIV diagnosis.
BMC Infect Dis. 2013 Oct 10;13:473.[
PMC free article: PMC3852490] [
PubMed: 24112129]
- 6.
Lally A, Casabonne D, Imko-Walczuk B, Newton R, Wojnarowska F. Prevalence of benign cutaneous disease among Oxford renal transplant recipients.
J Eur Acad Dermatol Venereol. 2011 Apr;25(4):462-70.[
PubMed: 20738465]
- 7.
Dessinioti C, Katsambas A. Seborrheic dermatitis: etiology, risk factors, and treatments: facts and controversies.
Clin Dermatol. 2013 Jul-Aug;31(4):343-351.[
PubMed: 23806151]
- 8.
Paulino LC. New perspectives on dandruff and seborrheic dermatitis: lessons we learned from bacterial and fungal skin microbiota.
Eur J Dermatol. 2017 Jun 01;27(S1):4-7.[
PubMed: 28690211]
- 9.
Honnavar P, Chakrabarti A, Prasad GS, Singh P, Dogra S, Rudramurthy SM. -Endorphin enhances the phospholipase activity of the dandruff causing fungi Malassezia globosa and Malassezia restricta.
Med Mycol. 2017 Feb 01;55(2):150-154.[
PubMed: 27497434]
- 10.
Turner GA, Hoptroff M, Harding CR. Stratum corneum dysfunction in dandruff.
Int J Cosmet Sci. 2012 Aug;34(4):298-306.[
PMC free article: PMC3494381] [
PubMed: 22515370]
- 11.
Sampaio AL, Mameri AC, Vargas TJ, Ramos-e-Silva M, Nunes AP, Carneiro SC. Seborrheic dermatitis.
An Bras Dermatol. 2011 Nov-Dec;86(6):1061-71; quiz 1072-4.[
PubMed: 22281892]
- 12.
Schwartz JR, Messenger AG, Tosti A, Todd G, Hordinsky M, Hay RJ, Wang X, Zachariae C, Kerr KM, Henry JP, Rust RC, Robinson MK. A comprehensive pathophysiology of dandruff and seborrheic dermatitis - towards a more precise definition of scalp health.
Acta Derm Venereol. 2013 Mar 27;93(2):131-7.[
PubMed: 22875203]
- 13.
Gaitanis G, Magiatis P, Hantschke M, Bassukas ID, Velegraki A. The Malassezia genus in skin and systemic diseases.
Clin Microbiol Rev. 2012 Jan;25(1):106-41.[
PMC free article: PMC3255962] [
PubMed: 22232373]
- 14.
Peyr J, Lleonart M., Grupo espaol del Estudio SEBDERM. [Clinical and therapeutic profile and quality of life of patients with seborrheic dermatitis].
Actas Dermosifiliogr. 2007 Sep;98(7):476-82.[
PubMed: 17669302]
- 15.
Augustin M, Kirsten N, Krber A, Wilsmann-Theis D, Itschert G, Staubach-Renz P, Maul JT, Zander N. Prevalence, predictors and comorbidity of dry skin in the general population.
J Eur Acad Dermatol Venereol. 2019 Jan;33(1):147-150.[
PubMed: 29953684]
- 16.
Hald M, Arendrup MC, Svejgaard EL, Lindskov R, Foged EK, Saunte DM., Danish Society of Dermatology. Evidence-based Danish guidelines for the treatment of Malassezia-related skin diseases.
Acta Derm Venereol. 2015 Jan;95(1):12-9.[
PubMed: 24556907]
- 17.
Victoire A, Magin P, Coughlan J, van Driel ML. Interventions for infantile seborrhoeic dermatitis (including cradle cap).
Cochrane Database Syst Rev. 2019 Mar 04;3(3):CD011380.[
PMC free article: PMC6397947] [
PubMed: 30828791]
- 18.
Cheong WK, Yeung CK, Torsekar RG, Suh DH, Ungpakorn R, Widaty S, Azizan NZ, Gabriel MT, Tran HK, Chong WS, Shih IH, Dall'Oglio F, Micali G. Treatment of Seborrhoeic Dermatitis in Asia: A Consensus Guide.
Skin Appendage Disord. 2016 May;1(4):187-96.[
PMC free article: PMC4908450] [
PubMed: 27386464]
- 19.
Das A, Panda S. Use of Topical Corticosteroids in Dermatology: An Evidence-based Approach.
Indian J Dermatol. 2017 May-Jun;62(3):237-250.[
PMC free article: PMC5448257] [
PubMed: 28584365]
- 20.
Kamamoto CSL, Nishikaku AS, Gompertz OF, Melo AS, Hassun KM, Bagatin E. Cutaneous fungal microbiome:
Malasseziayeasts in seborrheic dermatitis scalp in a randomized, comparative and therapeutic trial.
Dermatoendocrinol. 2017;9(1):e1361573.[
PMC free article: PMC5821162] [
PubMed: 29484095]
- 21.
Abbas Z, Ghodsi SZ, Abedeni R. Effect of itraconazole on the quality of life in patients with moderate to severe seborrheic dermatitis: a randomized, placebo-controlled trial.
Dermatol Pract Concept. 2016 Jul;6(3):11-6.[
PMC free article: PMC5006547] [
PubMed: 27648378]
- 22.
Skorvanek M, Bhatia KP. The Skin and Parkinson's Disease: Review of Clinical, Diagnostic, and Therapeutic Issues.
Mov Disord Clin Pract. 2017 Jan-Feb;4(1):21-31.[
PMC free article: PMC6174479] [
PubMed: 30363435]
- 23.
Schwartz JL, Clinton TS. Darier's disease misdiagnosed as severe seborrheic dermatitis.
Mil Med. 2011 Dec;176(12):1457-9.[
PubMed: 22338367]
- 24.
Prna E, Aluoja A, Kingo K. Quality of life and emotional state in chronic skin disease.
Acta Derm Venereol. 2015 Mar;95(3):312-6.[
PubMed: 24978135]
- 25.
Sanders MGH, Pardo LM, Ginger RS, Kiefte-de Jong JC, Nijsten T. Association between Diet and Seborrheic Dermatitis: A Cross-Sectional Study.
J Invest Dermatol. 2019 Jan;139(1):108-114.[
PubMed: 30130619]
Disclosure: Dan Tucker declares no relevant financial relationships with ineligible companies.
Disclosure: Sadia Masood declares no relevant financial relationships with ineligible companies.