What can be mistaken for seborrheic dermatitis
Psoriasis vs. Seborrheic Dermatitis: What You Should Know
Having an itchy, flaky scalp is a common problem for many people. However, before you can figure out how to treat the condition, you must identify the cause. Two conditions that can lead to an itchy scalp are psoriasis and seborrheic dermatitis:
- Psoriasis is a chronic skin disease. It can cause skin cells to grow so quickly that they accumulate on the surface of the skin. Patches of rough, scaly skin can appear anywhere on the body, including the scalp.
- Seborrheic dermatitis is a skin condition that can cause rough, scaly skin on the scalp and face. The common name for seborrheic dermatitis is dandruff. In babies, its called cradle cap.
Psoriasis tends to be pink or red with silvery scales on those with light or fair skin tones. On medium skin tones it can appear salmon-colored and silvery-white scales. On darker skin tones psoriasis tends to be violet with gray scales. Or it can also appear dark brown and difficult to see.
The patches can appear anywhere on the body, especially on the elbows and knees. They can also show up on the scalp. The patches can be itchy or tender to the touch.
Seborrheic dermatitis is usually found on the scalp, but it can sometimes appear elsewhere. It causes itchy patches of scaly skin that may look a little greasy but can flake, especially if you scratch.
Seborrheic dermatitis may look different in individuals with skin of color. It tends to be red and scaly on those with light or fair skin tones. On medium and dark skin tones this condition may appear as curved or petal-like lesions along the hairline. It can also cause hypopigmentation or lightening of the skin.
In babies, seborrheic dermatitis may be crusty. Children and babies of color tend to not experience the typical cradle cap appearance of seborrheic dermatitis. Instead they often have redness, a rash, flaking, and hypopigmentation of the affected areas and folds of skin often accompanied by atopic dermatitis.
Babies may also have seborrheic dermatitis around the eyes and nose. If the skin is scratched, theres some risk of bleeding or infection if the thick scale is picked or removed from the scalp.
Psoriasis and seborrheic dermatitis of the scalp share some common symptoms. They both result in:
- scaly patches of skin
- flakes that may attach to the hair shaft
- itching
How can you tell the difference? One clue is the scales. Psoriasis on the scalp on lighter skin tones often appears as red or pink and can have silvery-white scales. On darker skin tones, psoriasis is more likely to appear as dark or reddish brown or purple patches with overlying whitish or grayish scales.
The scales of seborrheic dermatitis are usually thinner. On lighter skin tones the scales are more likely to be pinkish-yellow with yellowish flakes, with a greasy appearance. In individuals with medium and dark skin tones, redness may be seen alongside flaking. Sometimes, the areas that are involved are lighter or darker than the individuals normal skin tone.
As for the patches, if you have psoriasis, its likely that you have them on other parts of your body. If you scratch or try to remove them, theyll probably bleed and also become thicker and itchier.
Seborrheic dermatitis patches are usually easy to remove, unless the pink patch which requires treatment. Psoriasis patches sometimes feel sore or tender, but seborrheic dermatitis doesnt.updated CSG
Its possible to have both scalp conditions at the same time.
Anyone can get psoriasis of the scalp. Theres no way to prevent it. Its more likely to occur in adults who have psoriasis elsewhere on their body.
The exact cause of psoriasis isnt known, but it involves an overreaction of the immune system. It tends to run in families, so its likely theres a genetic link.
Anyone can get seborrheic dermatitis, too. However, males develop it more often than females.
Some things that may play a role in developing seborrheic dermatitis include:
- a family history of seborrheic dermatitis
- oily skin
- using alcohol-based products
- weather extremes
- stress
- fatigue
Treatment may depend on the severity of your condition. Everyone responds differently to medication, so it may take a few tries to find the right solution for you.
Black, Indigenous, and People of Color patients may require a different treatment approach that takes into account differences in hair texture and hair washing frequency.
For some people, dandruff clears up on its own. Over-the-counter (OTC) shampoos and medication are usually enough to improve flaking and soothe itching. If not, ask your doctor about prescription-strength products.
In babies, cradle cap doesnt always require treatment. It generally resolves well before the first birthday. In the meantime, use a mild baby shampoo. Massage the scalp gently using a very soft brush. Be gentle breaking the skin can lead to infection. If youre concerned about your babys scalp, see their pediatrician.
MORE: Seborrheic Dermatitis: Best Shampoos for Treating Your Scalp
Psoriasis of the scalp may be harder to treat. Topical corticosteroids may help reduce inflammation and slow the growth of skin cells.
Psoriasis can also be treated with light therapy. Systemic treatment may be beneficial for stubborn psoriasis. This may involve oral treatments or injectable medications. It may take a combination of treatments to get psoriasis under control.
If you have a mild case of flaky skin on your scalp, OTC dandruff products may help. If they dont, have your doctor take a look. Also see your doctor if you have undiagnosed patches of skin that look abnormal in other places on your body.
Your doctor will likely be able to tell whether its psoriasis, seborrheic dermatitis, or something else just by examining your skin. It might take looking at a skin sample under a microscope to confirm a diagnosis. In rare cases, a biopsy is needed.
Both seborrheic dermatitis and psoriasis are chronic, lifelong conditions. But with a proper diagnosis, you can monitor and effectively manage them.
Seborrheic Dermatitis
Seborrheic dermatitis is a common form of eczema that usually affects the scalp, though it can affect other parts of the body as well.

While it rarely causes severe harm to the body, it can be uncomfortable to live with the constant itch, rash and other symptoms of seborrheic dermatitis. Fortunately, there are some effective treatment options and seborrheic dermatitis can sometimes go away on its own or with the right shampoo and skin care routine.
Lets dive into who gets seborrheic dermatitis, why it forms, common symptoms and treatment options.
What is seborrheic dermatitis?
Considered a chronic form of eczema, seborrheic dermatitis appears on the body where there are a lot of oil-producing (sebaceous) glands like the upper back, nose and scalp. It can cause a variety of symptoms from dandruff to a rash on the affected area.
For many infants and some adults, seborrheic dermatitis goes away on its own. If symptoms dont go away, there are many effective treatments to manage symptoms and stop seborrheic dermatitis flare-ups in the future.
Who gets seborrheic dermatitis and why?
Seborrheic dermatitis (also sometimes referred to as seborrhea or seborrhoeic dermatitis), can affect people of any age, though its most common in infants and adults between the ages of 30 and 60. Among adults and teens, this skin disease is more common in males.
In infants, this common skin condition usually clears on its own and doesnt come back. In adults, however, the prevalence of seborrheic dermatitis usually follows a pattern of flaring and clearing that can last for years.
Some research suggests 3-10 out of every 100 people will experience seborrheic dermatitis in their lifetime. Many folks who get seborrheic dermatitis as a young adult or after 50 suffer from chronic seborrheic dermatitis and they experience flare-ups throughout their life.
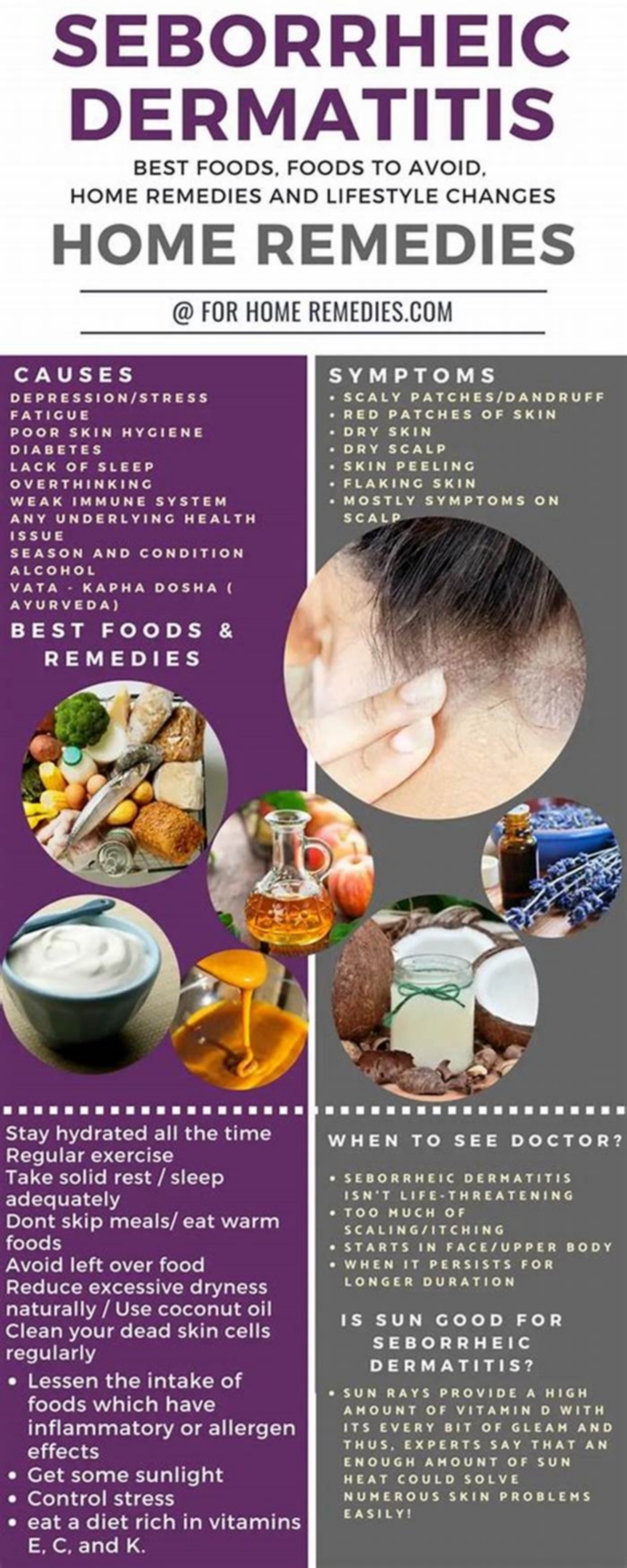
What causes seborrheic dermatitis?
Seborrheic dermatitis is usually caused by a combination of genetic and environmental factors.
The trigger is usually an inflammatory reaction to excess Malassezia yeast, also sometimes called pityrosporum. This organism that normally lives on the skins surface, is the likely cause of seborrheic dermatitis. The Malessezia overgrows and the immune system seems to overreact to it, leading to a fungal infection that results in skin changes.
Certain medical conditions can increase peoples risk of developing seborrheic dermatitis, including psoriasis, HIV, acne, rosacea, Parkinsons disease, epilepsy, alcoholism, depression, eating disorders and recovery from a stroke or heart attack.
Common triggers for seborrheic dermatitis include:
- stress
- recovery from a stressful life event, like losing a loved one or a heart attack
- hormonal changes or illness
- harsh detergents, solvents, chemicals and soaps
- cold, dry weather or a change in the season
- some medications, including psoralen, interferon and lithium
- certain medical conditions, such as HIV and Parkinsons disease
Like all forms of eczema, seborrheic dermatitis is not contagious. You cannot catch it from another person. Instead, its the result of environmental and genetic factors.
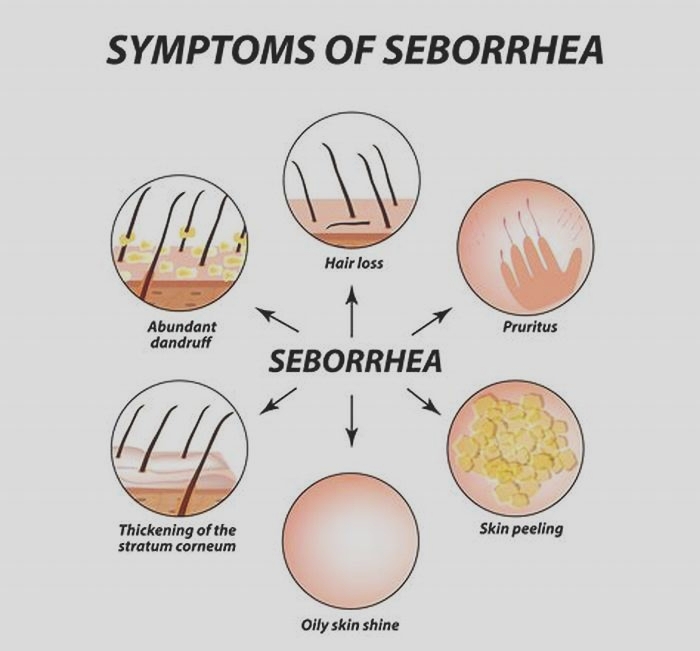
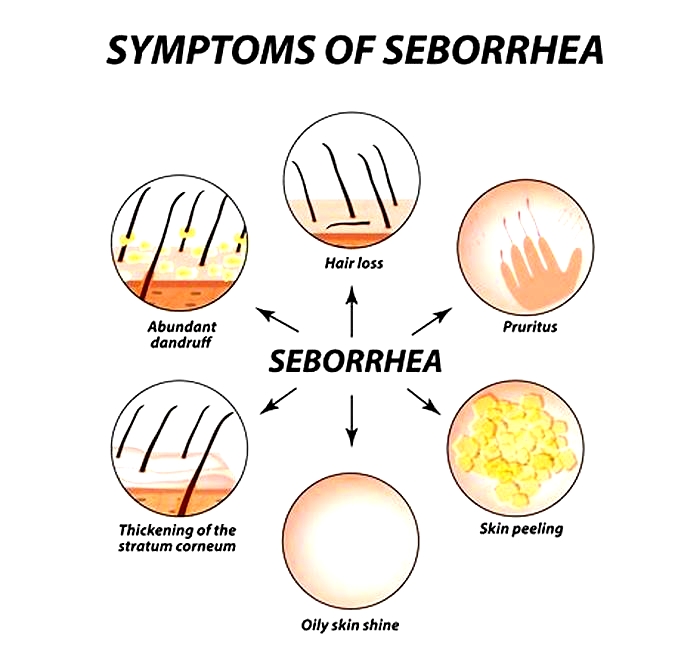
What are the symptoms of seborrheic dermatitis?
Seborrheic dermatitis can be the culprit for a variety of symptoms depending on age, race, and the severity of a flare-up. Sometimes, symptoms will go away on their own or with changes in your skincare and hair regimens.
Seborrheic dermatitis and cradle cap in infants
Infants with seborrheic dermatitis most often have a form called cradle cap, which appears on their scalps as scaly, greasy patches. Infants can also develop seborrheic dermatitis on their bottoms, where it can be mistaken for diaper rash, a form of contact dermatitis.
Seborrheic dermatitis in adults and adolescents
When seborrheic dermatitis appears near the scalp in adults and adolescents, its often referred to as facial seborrheic dermatitis. Common symptoms of facial seborrheic dermatitis include inflamed skin and itching.
With this form, symptoms might also appear on the eyelids, on the sides of the nose, in and around the eyebrows and near the ears. Facial seborrheic dermatitis can also cause stubborn dandruff. But seborrheic dermatitis doesnt just form on the face. It can appear in oily skin all over the body. In addition to the face, redness, swelling and greasy scaling can develop on the mid-chest, upper back and in the armpits, under the breasts and in the groin area.
Common symptoms
No matter where seborrheic dermatitis is on the body, there are common symptoms experienced by many with this condition. These symptoms include:
- Flaking skin or dandruff;
- Patchy of flaky white or yellow scales on top of greasy skin;
- A irritable rash which looks dark in brown and Black skin and lighter in white skin;
- Ring-shaped rash for those with petaloid seborrheic dermatitis;
- Itchiness.
The affected skin sometimes crusts over and lesions containing sebum can form. Erythema, or redness of the skin caused by inflammation, may also be experienced. If the flare-ups occur in creases in the hairline, those who itch the affected areas too much may experience hair loss as well.
African Americans and those with skin of color might experience petaloid seborrheic dermatitis, a more severe form where lesions form around the hairline and skin discoloration happens. Usually, the discolored skin manifests in a ring-shaped rash. When looking more generally at the relationship between eczema and skin of color, itching due to eczema has been shown to have a greater impact in Black patients, who are also more likely to have severe disease.
Symptoms of severe cases
More severe cases can lead to the immunodeficiency of affected skin and an increased risk for infections. Seborrheic dermatitis is not precancerous. If you have this form of eczema, it does not increase your chance of getting skin cancer.
Another common misconception is that seborrheic dermatitis leads to hair loss. This is completely false. Hair loss is not a symptom of seborrheic dermatitis and if you are experiencing hair loss, you probably have a different underlying condition.
Whether your severe symptoms are from seborrheic dermatitis or something else, its best to visit an experienced healthcare provider, such as a dermatologist. This healthcare provider can help you get your severe symptoms under control so they stop disrupting your daily life.
How is seborrheic dermatitis treated?
Depending on the severity of the case, you might be able to treat this form of eczema with a shampoo swapor seborrheic dermatitis might even go away without treatment. If symptoms persist for longer than two weeks, you probably want to consider talking to a healthcare provider about over the counter and prescribed treatment options. Most adults with this condition will need a treatment plan to manage symptoms.
Use the right shampoo and skincare products
Following a skincare routine can help keep symptoms under control. Wash affected areas daily with a gentle, zinc-containing cleanser (2% zinc pyrithione) and follow up with a lotion or moisturizer.
If the hairline is affected, consider a dandruff shampoo and hair products designed for sensitive skin. Some of the best non prescription dandruff shampoos include those with:
- Pyrithione zinc. Selenium sulfide;
- Ketoconazole 1%;
- Tar;
- Salicylic acid.
Popular brands with one or more of these active ingredients include DermaZinc, Head & Shoulders, Selsun Blue, Nizoral and Denorex Extra Strength.
For more on the best products for infants with cradle cap, adolescents, and adults with seborrheic dermatitis, check out our list of products with the NEA Seal of AcceptanceTM.
Lifestyle changes
Healthy lifestyle habits, like managing stress and getting plenty of sleep, can also improve skin. Stress relief is often the lifestyle change which will have the biggest impact on seborrheic dermatitis. Some particularly effective stress relief techniques include:
- Perform light exercise, such as yoga or a gentle walk;
- Journal about stress and negative feelings;
- Develop a mediation or breathwork practice;
- Spend time in nature, even if its just five minutes.
There are many other ways you can reduce stress. What matters most is finding an enjoyable technique that allows you to slow down and devote time to self care.
Over the counter treatments and medicated shampoo
If lifestyle and skin care routine changes dont work, it might be time to consider over the counter (OTC) and prescription options. OTC and prescription treatment for this skin disorder is aimed at removing scales, reducing itch and calming the inflammation thats causing redness and swelling.
In infants, using an emollient such as mineral oil or petroleum jelly, to gently loosen scales is usually all thats needed. Care can be more complicated for adults, who often need ongoing treatment and self-care to help prevent flare-ups.
Dermatologists usually begin treating mild cases with a topical antifungal cream or medicated shampoo, such as a prescription anti-fungal shampoo or over-the-counter dandruff product.Some popular topical treatments include creams with 1% ciclopirox or 2% ketoconazole. Because both ciclopirox and ketoconazole can dry out the skin, its important to use a gentle moisturizer after applying a cream with either ingredient.
Prescribed treatments
If the condition is more severe, intermittent use of a topical corticosteroid like fluocinolone, dermatol, additional steroids or calcineurin inhibitor may be required. Other treatments for severe cases include hydrocortisone ointments or oral medications, such as pimecrolimusor tacrolimus.
Make sure to talk to a dermatologist or another healthcare provider who is experienced in dermatology about options for the treatment of seborrheic dermatitis and the side effects of each option.
When to see a healthcare provider
If youre considering over the counter or prescription options, you will want to discuss the best path with a doctor. It might also be a good idea to discuss any lifestyle changes or skin and hair products with a healthcare provider before taking them.
You should also see your healthcare provider if you experience a severe flare-up or have worse symptoms than usual. In this case, your doctor can help you change your medication dose or switch to a different treatment option.
After talking to your healthcare provider, they may order a skin biopsy. This is when a small piece of your skin is removed in order to be studied in a lab. The skin biopsy can help your healthcare provider determine if this is seborrheic dermatitis or something else and the best treatment plan moving forward.
Whether they order a skin biopsy or not, it will most likely be useful to discuss your seborrheic dermatitis with your doctor. During an appointment, your healthcare provider might ask you:
- How long have you had symptoms? What are your current and past symptoms?
- What treatment options have you tried and how have they worked?
- What treatment options are covered by my insurance?
- How often should we meet to monitor my seborrheic dermatitis?
After your healthcare provider gathers the answers to these questions, examines the affected areas, and possibly orders a skin biopsy, they should have customized recommendations on how to create a treatment plan moving forward.
What do the ecz-perts have to say?
Seborrheic dermatitis isnt contagious and is not an allergy, although some allergies can mimic it, said Dr. Peter Lio, clinical assistant professor of dermatology and pediatrics at Northwestern Universitys Feinberg School of Medicine. A correct diagnosis, he added, requires careful evaluation by a dermatologist.
Seborrheic dermatitis can also overlap with atopic dermatitis, especially in infants. We see this overlap in young adults, as well, usually in those with more severe atopic dermatitis, Lio said. They can develop a condition that some call head and neck dermatitis that seems to be very closely related to seborrheic dermatitis and is treated similarly.
In conclusion
If you are experiencing seborrheic dermatitis, theres no need to fret. While the symptoms can be irritating, there are many effective treatment options out there. After a conversation with a healthcare professional, you should be able to develop a treatment plan for even the most severe case.