What does a fungal rash look like on dogs

Fungal Dermatitis in Dogs: Signs, Symptoms & Treatments
What is fungal dermatitis in dogs?
Fungal dermatitis is also known as a yeast infection or Malessezia dermatitis, as its caused by the fungus Malessezia pachydermatis.
This fairly common inflammatory skin condition is referred to as a yeast infection, and can occur when the yeast that normally lives in your pets ears, mucocutaneous areas and skin reproduces uncontrollably and overpopulates these areas.
What causes fungal skin infections?
We know that yeast thrives in hot, humid environments, and infections can happen if your pets immune system is compromised or if they are taking strong immunosuppressive drugs. An increase in the amount of oils produced on the skin, or excess skin oils, can cause the condition.
Other yeast-like organisms or fungi may invade the circulation system and cause issues in your dogs organs. These more serious fungi can include histoplasmosis, cryptococcus and Valley Fever, among others.
Fortunately, fungal dermatitis is not contagious, but can recur unless the underlying skin condition or allergy is controlled with medication.
As for which breeds are predisposed to yeast infections, be on guard if youve got a Cocker Spaniel, Shetland Sheepdog, Dachshund, Basset Hound, West Highland White Terrier, Silky Terrier, Maltese Terrier, Australian Terrier, Poodle, or Lhasa Apso.
What are signs and symptoms of fungal dermatitis?
When harmless malassezia changes to a pathogenic form, it can become problematic and result in symptoms such as:
- Skin irritation
- Inflammation
- Intense itchiness
- Flaky, crusty or scaly skin
- Thickened/elephant skin
- Ear infections
You may especially notice these signs between your four-legged friends paw pads and nails, and on the neck, nasal folds, armpits and anal area. Also check around his years. Secondary symptoms can include a sticky discharge, skin redness or sores.
Your dogs coat is often a good indicator of their overall health, and thats also true in cases of yeast infection; if her coat is greasy or there are signs of hair loss, or foul-smelling skin, she should see a vet.
How is fungal dermatitis in dogs diagnosed?
Your vet may use any of these techniques to collect a sample from your dog so his infection can be diagnosed and treated:
Skin biopsy - The most invasive diagnostic test uses a biopsy punch to obtain a small piece of skin. However, this provides the most complete diagnostic data.
Cotton swab sample - The skin is rubbed with a moistened swab to collect yeast organisms. Impression smear - A microscope slide is pressed onto the skin to collect yeast organisms. Acetate tape preparations - A piece of clear tape is applied to the skin to collect yeast organisms.
Skin scrape - The skin is scraped with a blade so yeast organisms can be collected.
How is fungal dermatitis treated?
There are a number of options for treating yeast infections in dogs, including oral or topical solutions. Sometimes your vet will prescribe a combination of both if the case is severe.
Oral Treatment
This type of treatment would be used for persistent, severe or chronic cases of yeast dermatitis. Bacterial skin infections can also accompany the condition and require 4 to 12 weeks of antibiotics. Systemic anti-fungal medications are often in this category and can include itraconazole, fluconazole and ketoconazole.
Use caution with these because although they are highly effective, these drugs can have potential side effects for your dogs liver. Routine blood tests and close monitoring are a must.
Topical Treatment
An essential step to treating yeast dermatitis is to use a medicated shampoo containing benzoyl peroxide or selenium sulfide. After a first degreasing cleansing session has taken place with the shampoo, taking at least a 10-minute bath with an anti-fungal shampoo is recommended. Effective topical treatments are needed every 3 to 5 days for 2 to 12 weeks to eradicate the infection.
If an infection is diagnosed on the ears or on just one or two isolated spots on the skin, your dog may require a topical ointment for daily use.
What is the prognosis for treating fungal dermatitis?
Yeast infections can generally be treated long-term and you may see less itching within a week of starting the prescribed treatment.
If your dog has an underlying issue such as a compromised immune system or allergy, how well these conditions can be treated and controlled will determine the outcome. Some dogs will experience secondary yeast or bacterial skin infections along with severe skin allergies - sometimes two to three times each year.
If this is the case, your veterinarian can develop a custom treatment plan for your dog to help manage the condition.
Do you suspect your pet has fungal dermatitis? Our Greensboro vets have experience with treating a number of conditions, allergies and illnesses in dogs. Contact us today.
Everything You Want to Know About Ringworm
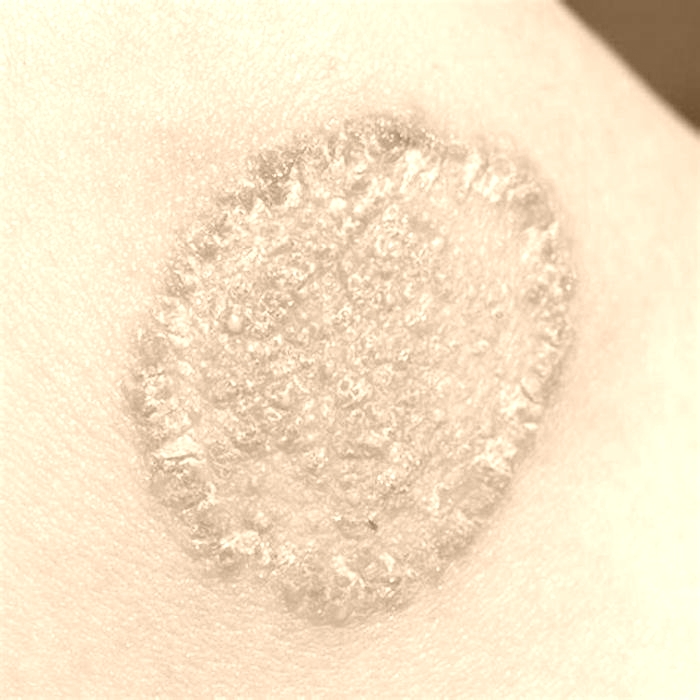
Ringworm is a fungal infection that causes a ring-shaped infection on the skin. Conditions like eczema and psoriasis can sometimes resemble ringworm, but there are key differences in appearance and treatment.
Ringworm also known as dermatophytosis, dermatophyte infection, or tinea is a fungal infection of the skin.
Read on to learn how to recognize when you have ringworm, its symptoms, causes, treatment, and more.
Ringworm is actually a misnomer since its a fungus and not a worm that causes the infection. The lesion caused by this infection resembles a worm in the shape of a ring, which is why it got its name.
Ringworm is usually specifically used to describe tinea corporis (ringworm of the body) or tinea capitis (ringworm of the scalp). Its sometimes used to describe tinea infection in other locations, such as tinea cruris (ringworm of the groin).
Ringworm initially appears as discolored, often scaly patches on affected areas. These patches typically appear red on lighter skin or brown-gray on darker skin.
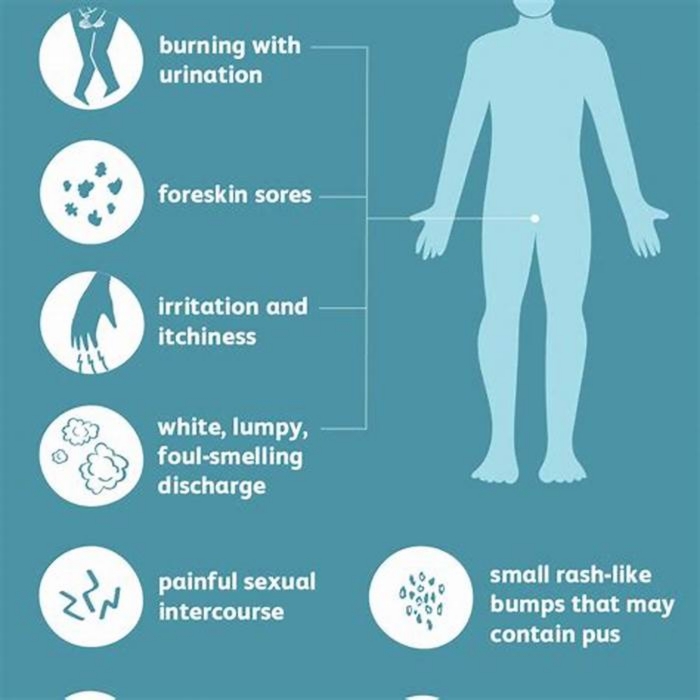
Symptoms vary depending on where the infection occurs. With a skin infection, you may experience the following:
- itchiness
- itchy or scaly patches that are red, brown, or gray, or raised areas of skin called plaques
- a round, flat patch of itchy skin
- patches that develop blisters or pustules
- patches that resemble a ring with deeper color on the outside
- patches with edges that are defined and raised
- overlapping rings
- hair loss
Symptoms by type
Ringworm can look different depending on which part of the body is affected. Doctors call ringworm different names depending on where it appears on the body.
- Ringworm of the body: Tinea corporis often appears as patches with the characteristic round ring shape on your torso or limbs.
- Ringworm of the scalp: Tinea capitis often starts as isolated scaling in the scalp that develops into itchy, scaly bald patches. Its most common among children. Hair around the affected area may break or fall off, and bald patches may develop.
- Ringworm of the beard: Tinea barbae affects your cheeks, chin, and upper neck and can cause bald patches. This may look like acne, folliculitis, or another skin condition. Some people experience fatigue or swollen lymph nodes.
- Ringworm of the hand: Tinea manuum is usually caused by touching another affected area, such as your groin or foot. Infection of the hand may look like very dry skin with deep cracks on the palm. If the infection spreads, you may see ring-shaped patches on the back of your hand.
- Jock itch: Tinea cruris is a ringworm infection of the skin around the groin, inner thighs, and buttocks. Its
most common in men and adolescent boys. It usually starts as an itchy red, brown, or gray rash where your leg and body meet. The itching may intensify after exercise and may not improve after using an anti-itch cream such as a steroid cream. The steroid cream could actually worsen the jock itch rash. - Athletes foot: Tinea pedis is a ringworm infection of the foot. Its frequently seen in people who walk barefoot in public places where the infection can spread, such as locker rooms, showers, and swimming pools. This starts as dry scaly skin between your toes that may spread to your sole and heel and leads to symptoms like itching, stinging, burning, as well as blistering or peeling skin, along with a foul odor.
- Tinea unguium: This is a type of fungal ringworm infection of the nails. It affects toenails more than fingernails, as footwear often provides a moist, warm environment that fungi prefer. The affected nails may become thicker or discolored. They may even begin to crack or lift away from your nail bed.
Symptoms by stage
You wont see ringworm right away when you first pick up the fungus. It can take up to 3 weeks before you start noticing symptoms. Some of the stages you may see include:
- Initial stage: During this stage, you may notice a discolored, irritated patch of skin. Sometimes, it just appears very dry and scaly, not necessarily like ringworm.
- Second stage: During this stage, youll notice the lesion starts to grow in size. The center of the rash may resemble healthy skin with a surrounding scaly area.
Its important to start treatment at the first signs of a ringworm infection. If you dont, it may spread and grow.
About
These fungi can live on your skin and other surfaces, particularly damp areas. They may also live for an extended period of time as spores in the soil.
Is ringworm contagious?
Ringworm fungi are very contagious and can spread to humans in four ways:
- Human to human: You can get the infection if you come in contact with a person who has ringworm or if you share personal items, such as combs or towels. The infection is commonly spread among children and by sharing items harboring the fungus.
- Animal to human: You can get ringworm after touching an affected animal or even items the animal has come in contact with. Cats and dogs are
common sources , but other animals, such as farm animals, can spread fungi as well. The animals pick up the fungus spores from the environment, and the spores transfer to whatever the animals hair touches. According to the American Kennel Club, cats are more prone to getting ringworm than dogs. - Object to human: You may get the infection if you come in contact with an object or surface that has it, such as a telephone or the floor of a public shower. These fungi thrive in damp environments.
- Soil to human: Humans and animals can get ringworm after direct contact with soil that is carrying the fungi.
Ringworm is
Will ringworm go away on its own?
Ringworm could go away on its own, but its likely to take longer than with treatment and is more likely with milder cases. Learn more about the length of contagion for ringworm.
Your doctor may give you a diagnosis of ringworm after examining your skin and possibly using a black light to view the affected area. Depending on the type of fungus, it may sometimes fluoresce (glow) under black light.
Your doctor may confirm a diagnosis of ringworm by requesting certain tests:
- If youre getting either a skin biopsy or fungal culture, your doctor will take a sample of your skin or discharge from a blister and send it to a lab to test for the presence of fungus.
- If youre getting a KOH exam, your doctor will scrape off a small area of affected skin onto a slide and place drops of a liquid called potassium hydroxide (KOH) on it. The KOH breaks apart typical skin cells, making the fungal elements easier to see under a microscope.
The treatment will depend on the type of ringworm you have and what part of your body it affects.
Medications
Your doctor may prescribe topical or oral antifungals depending on the severity of your ringworm infection and what part of your body it affects.
They may also recommend OTC medications and antifungal creams containing clotrimazole, miconazole, terbinafine, or related ingredients.
While getting treatment, make sure to wash your bedding and clothing daily to help disinfect your surroundings. Dry your skin thoroughly after bathing and wear only loose clothing in the affected areas.
Take an in-depth look at ringworm treatments.
Home remedies
People have long used home remedies for ringworm such as apple cider vinegar, coconut oil, turmeric, and certain essential oils.
However, these treatments are not scientifically proven, so its a good idea to consult a doctor before trying them. Home remedies shouldnt replace known antifungal treatments.
Learn more about home remedies for ringworm.
Treatment during pregnancy
If you get ringworm during pregnancy, there are topical medications
These drugs arent known to cause problems for a baby. However, consult your doctor before using any medications while pregnant. Doctors usually dont recommend oral medications like ketoconazole and miconazole due to their potential side effects during pregnancy.
You should also talk with your doctor before using any medications if youre breastfeeding or chestfeeding.
Anyone can get ringworm, but you may be
- live in a warm, humid environment or climate
- participate in contact sports, like wrestling or football
- use public showers or locker rooms
- come in close contact with animals
- wear tight shoes or clothes that chafe your skin
- have diabetes
- have obesity or are overweight
- sweat excessively
- have a weakened immune system
- go barefoot in public showers or pools
Practicing healthy and hygienic behaviors can help prevent ringworm. Infections may come from contact with animals and lack of hygiene. Several tips to prevent ringworm include:
- washing your hands after interacting with an animal
- disinfecting and cleaning pet living areas
- limiting contact with people or animals with ringworm if you have a weakened immune system
- wearing shoes if showering or walking in community areas
- not sharing personal items like clothing, towels, or hairbrushes with people who might have ringworm
- changing your socks and underwear at least once a day
- keeping your gear and uniform clean if you play sports
- keeping your skin clean and dry
To reduce the chance of transmission, its also important to avoid prolonged water exposure in public showers orpools because wet skin can make you more susceptible to infection.
If left untreated, ringworm can spread to other areas of your body. You may also risk spreading the infection to someone else. Other potential complications include:
- hair loss and scarring
- dark marks left on your skin, particularly on darker skin
- nail deformities
- secondary infection if any bacteria entered broken skin
- Majocchis granuloma a rare infection where the fungus has made its way to deeper layers of the skin
The complications of tinea capitis can be worrisome because it can produce lifelong permanent hair loss. When considering these potential complications, its best to treat ringworm as quickly as possible.
Two skin conditions can resemble ringworm. They are:
- Nummular eczema: This kind of eczema is similar to ringworm because it also causes round or coin-shaped lesions on your skin. Often, the only way to tell the difference is to have your doctor take samples of the skin cells and send them to a laboratory for testing.
- Plaque psoriasis: This is a disorder causing inflammatory plaques on your skin. Small, isolated plaques can sometimes look similar to ringworm.
Learn more about the differences between ringworm, nummular eczema, and psoriasis.
Skin medications may clear ringworm on your torso and limbs in 24 weeks.
If youre experiencing severe dermatophytosis that isnt responding to OTC treatments or home remedies, or if you suspect a tinea infection of your scalp or hair follicles, your doctor may prescribe antifungal pills to clear up the infection.
Most people respond positively to treatment.