What makes seborrhea worse
Seborrheic dermatitis: Self-care
 Biosimilars: 14 FAQs
Biosimilars: 14 FAQsFind answers to questions patients ask about this newer treatment option, including, Whats involved in switching from a biologic to a biosimilar?
Featured
 Laser hair removal
Laser hair removalYou can expect permanent results in all but one area. Do you know which one?
 Scar treatment
Scar treatmentIf you want to diminish a noticeable scar, know these 10 things before having laser treatment.
 Botox
BotoxIt can smooth out deep wrinkles and lines, but the results arent permanent. Heres how long botox tends to last.
Featured
 Find a Dermatologist
Find a DermatologistYou can search by location, condition, and procedure to find the dermatologist thats right for you.
 What is a dermatologist?
What is a dermatologist?A dermatologist is a medical doctor who specializes in treating the skin, hair, and nails. Dermatologists care for people of all ages.
Seborrheic Dermatitis
Seborrheic Dermatitis
What is seborrheic dermatitis?
Seborrheic dermatitis is a common type of rash. It causes red, scaly, greasy skin. It occurs on skin that has oil glands, such as the face, scalp, ears, back, and upper chest. A common type of scalp seborrheic dermatitis is dandruff. It tends to last a long time, or go away and come back. It is often made worse by cold weather, hormonal changes, and stress. Seborrheic dermatitis is not spread from person to person.
How to say it
seh-boh-REE-ihk der-mah-TI-tihs
What causes seborrheic dermatitis?
The cause is not yet known. It may be partly caused by your bodys response to a type of yeast that grows on skin, along with extra oil production. Experts are still learning more. Seborrheic dermatitis may run in families.
Who is at risk for seborrheic dermatitis?
Seborrheic dermatitis is very common and can be found in anyone at any age. But it's even more frequent in:
Men
People with oily skin or hair
People with HIV/AIDS, Parkinson disease, alcoholic pancreatitis, hepatitis, or cancer
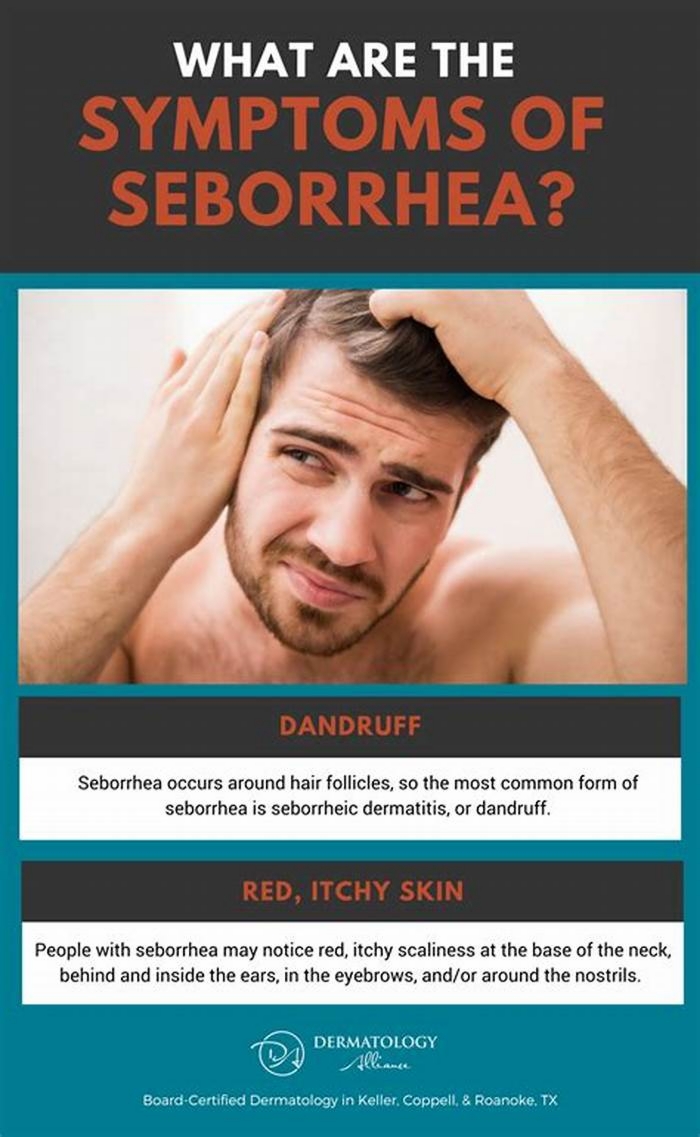
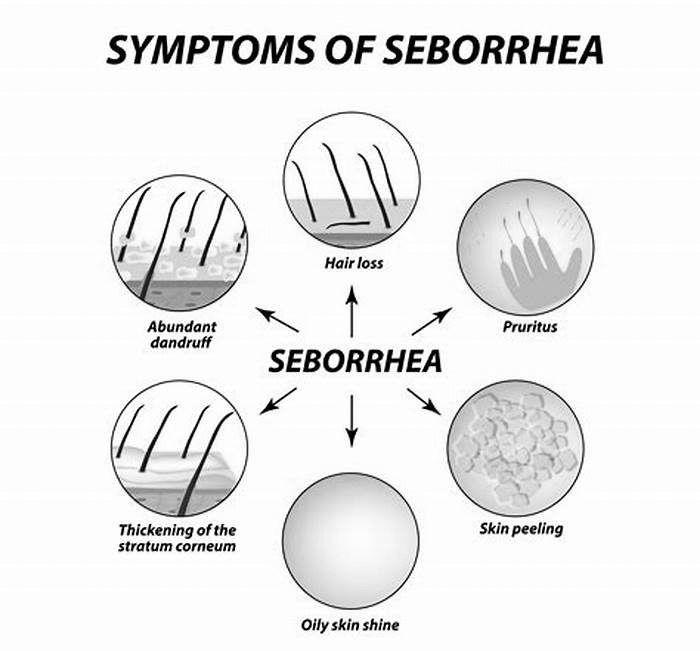
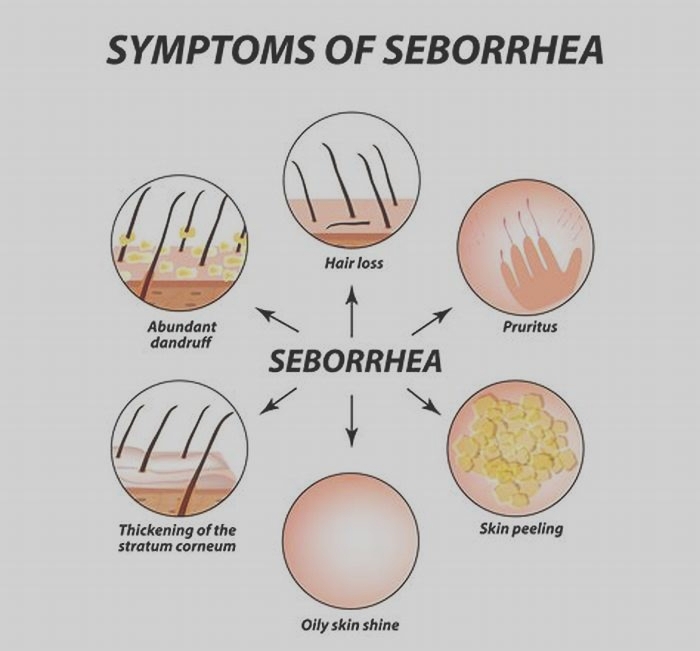
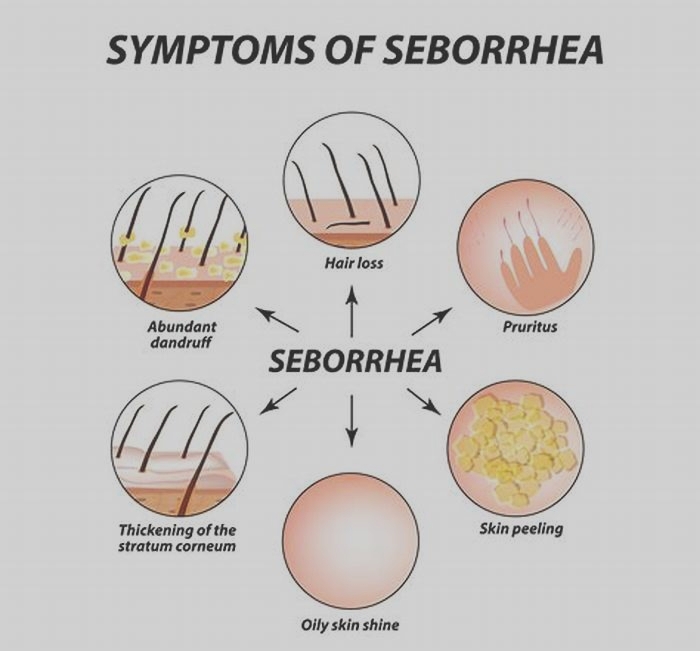
What are the symptoms of seborrheic dermatitis?
Symptoms can occur a bit differently in each person. They can include skin that is:
Bumpy
Covered with flakes (dandruff on the scalp, eyebrows, facial hair)
Covered with yellow scales or crusts
Cracked
Greasy
Itchy
Leaking fluid
Painful
Red or orange
These symptoms can occur on skin:
The symptoms of seborrheic dermatitis can be like other health conditions. Make sure to see your healthcare provider for a diagnosis.
How is seborrheic dermatitis diagnosed?
Your healthcare provider will ask about your symptoms and health history. They may also ask about your familys health history. They will give you a physical exam. The physical exam will include looking closely at your rash. Your provider may do a biopsy, but this is usually not needed.
How is seborrheic dermatitis treated?
Treatment will depend on your symptoms, your age, and your general health. It will also depend on how severe the condition is.
Treatment can reduce symptoms. Treatments often include:
Antifungal shampoo, body wash, or cream. These contain medicines such as ketoconazole, fluconazole, selenium sulfide, or ciclopirox.
Corticosteroid cream or ointment. These contain medicines such as hydrocortisone or fluocinolone acetonide.
Calcineurin inhibitor cream or ointment. These contain medicines such as pimecrolimus or tacrolimus.
Shampoo or cream with other medicines. These contain medicines such as coal tar, salicylic acid, or zinc pyrithione.
Sodium sulfacetamide creams and washes. These may also help reduce symptoms.
It's common for one medicine to work for many months, then stop working for a while. Switching to another medicine will often work. Many people rotate between therapies every few months to remain clear.
Talk with your healthcare providers about the risks, benefits, and possible side effects of all medicines.
What can I do to prevent seborrheic dermatitis?
Researchers dont know how to prevent seborrheic dermatitis.
How to manage seborrheic dermatitis
Seborrheic dermatitis is an ongoing (chronic) condition. It can go away and then come back. You will likely need to use shampoo, cream, or ointment with medicine once or twice a week. This can help to keep symptoms from coming back or getting worse. Wash your skin gently. You can remove scales with oil and gentle rubbing or a brush.
When should I call my healthcare provider?
Call the healthcare provider if you have:
Severe, thick scales on your scalp
Symptoms that dont get better, or get worse
New symptoms
Key points about seborrheic dermatitis
Seborrheic dermatitis is a common type of rash. It causes red, scaly, greasy skin. It occurs on skin that has oil glands, such as the face, scalp, and upper chest.
It tends to last a long time, or go away and come back. It is often made worse by cold weather, hormonal changes, and stress.
Symptoms can include skin that is bumpy, scaly, greasy, and itchy.
Treatment such as medicine in shampoo, body wash, and lotion can reduce symptoms.
Seborrheic dermatitis is an ongoing (chronic) condition. It can go away and then come back. You will likely need to use shampoo, cream, or ointment with medicine once or twice a week.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
Know the reason for your visit and what you want to happen.
Before your visit, write down questions you want answered.
Bring someone with you to help you ask questions and remember what your provider tells you.
At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
Know why a new medicine or treatment is prescribed and how it will help you. Also know what the side effects are.
Ask if your condition can be treated in other ways.
Know why a test or procedure is recommended and what the results could mean.
Know what to expect if you do not take the medicine or have the test or procedure.
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
Know how you can contact your provider if you have questions.
Seborrheic Dermatitis: A Dermatologist Talks Treatment
What is seborrheic dermatitis?
 Seborrheic dermatitis is a common skin condition that affects the areas of the body that have a high density of oil-producing (sebaceous) glands.
Seborrheic dermatitis is a common skin condition that affects the areas of the body that have a high density of oil-producing (sebaceous) glands.
It affects 1 to 5 percent of the general population, and often has a chronic, relapsing course.
The exact cause of seborrheic dermatitis is not completely clear, although genetic and hormonal influences have been shown to play a role in this condition. Furthermore, certain fungal microorganisms that live naturally on the skin, belonging to the genus Malassezia, can also contribute to seborrheic dermatitis.
Patients of any age can develop seborrheic dermatitis, including infants (in which it is known as cradle cap), teenagers, and adults.
Flares of seborrheic dermatitis have been associated with many factors, such as stress, hormonal changes, or illness. Skin irritants such as certain detergents, solvents, chemicals, and soaps may also worsen seborrheic dermatitis. In general, seborrheic dermatitis is slightly more common in men than in women. Patients with certain diseases that affect the immune system (such as HIV/AIDS) and the nervous system, such as Parkinsons disease, are also at increased risk of developing seborrheic dermatitis.
Seborrheic dermatitis mainly affects the scalp, where it may range from dry flakes (dandruff) to yellow, greasy scales with reddened underlying skin. Patients can also develop seborrheic dermatitis on other oily areas of their body, such as the face, upper chest and back. Seborrheic dermatitis is not harmful to a patients health, nor is it contagious, and fortunately complications are rare. It can, however, have a profound impact on a patients quality of life and emotional well-being.
How can you identify it?

Example of seborrheic dermatitis on the face. Photo courtesy of Skinsight.com, Logical Images, Inc.
Seborrheic dermatitis can often resemble other skin conditions. The typical symptoms that patients with seborrheic dermatitis experience include redness, flaking, scaly patches, and sometimes itching of the affected skin. Like eczema and psoriasis, two other common skin diseases, seborrheic dermatitis produces inflammation of the skin.
Seborrheic dermatitis can look like and/or overlap with other skin conditions. If you are experiencing symptoms, it is important to see a dermatologist to get the correct diagnosis and treatment. There is no specific test for diagnosing seborrheic dermatitis. Your dermatologist will ask about your medical history and also perform a physical examination of your skin. Usually, these measures alone will be sufficient to make the diagnosis.
In certain cases, a scraping of skin under a drop of potassium hydroxide is examined under a microscope to exclude a fungal infection. Similarly, a skin biopsy (a procedure in which a small sample of skin is removed) may be required in rare cases to confirm the diagnosis or rule out other conditions that mimic seborrheic dermatitis.
How is seborrheic dermatitis different from atopic dermatitis?

Example of seborrheic dermatitis on the chest. Photo courtesy of Skinsight.com, Logical Images, Inc.
Atopic dermatitis and seborrheic dermatitis are both forms of eczema, a general term that describes inflammatory skin conditions that produce significant redness and itching. Not uncommonly, a single person can be diagnosed with both seborrheic dermatitis and atopic dermatitis. Atopic dermatitis nearly always produces itchy, red skin but seborrheic dermatitis is not always itchy. The areas of affected skin can also differ between both of these conditions. Distinct from seborrheic dermatitis, atopic dermatitis most often affects the face, hands, feet, inside of the elbows and behind the knees.
Additionally, Malassezia organisms are known to contribute to seborrheic dermatitis. As a result, the treatment approaches to atopic dermatitis and seborrheic dermatitis are different.
Topical medications such as steroids, pimecrolimus, and tacrolimus are traditionally used to help relieve symptoms of atopic dermatitis. But for seborrheic dermatitis, the treatments instead target fungi that like oil glands, like Malassezia.
Nonetheless, distinguishing between seborrheic dermatitis and atopic dermatitis can pose a challenge even for healthcare professionals, and it is therefore important to see a physician should you develop concerns about your skin.
How is seborrheic dermatitis treated?
The symptoms of seborrheic dermatitis can be effectively controlled, and currently a variety of medicated treatments are available both over the counter and by prescription. A combination of self-care measures and drug therapy is often required to optimally treat seborrheic dermatitis.
For adults, long-term maintenance may be necessary to control the symptoms of seborrheic dermatitis. Dandruff, which represents mild seborrheic dermatitis of the scalp, may be treated with over-the-counter anti-dandruff shampoos. These contain one of several available active ingredients: selenium sulfide, tar, zinc pyrithione, and ketoconazole. These have all been shown to be equally effective after four weeks of consistent use.
Antifungal solutions containing ketoconazole, such as the shampoo Nizoral, are considered mainstays of treatment because they kill fungi such as Malassezia. For best results, shampoos should be left in place for five to ten minutes before rinsing, and then rinsed out completely. Initially, medicated shampoos may be used every day, and then as symptoms improve, they can be tapered to every other day. If one shampoo does not improve symptoms after four to six weeks, then a different shampoo may be tried.
For seborrheic dermatitis affecting areas other than the scalp, topical steroids such as hydrocortisone can also alleviate the redness and itching. These may be applied once or twice daily for up to two weeks. Very rarely, a systemic medication (often in the form of a pill), such as an antifungal medication or steroid, may be required to control symptoms if they are severe.
Fortunately, although there is no permanent cure yet, seborrheic dermatitis often improves with an excellent response once treatment is started.
Ultimately, however, it is important to note that if symptoms fail to improve with therapy or worsen, then you should make an appointment with a health care provider to have your symptoms evaluated further.
Conclusion
In conclusion, seborrheic dermatitis is a condition that can be readily managed with a balance of self-care and medicated treatments. Patients experience improvement and flares intermittently throughout their disease course, which tends to be chronic.
Factors such as hormones, genes, exposures to chemicals, and stress can all potentially trigger flares of seborrheic dermatitis.
For overall health, it is also important to consult with your physician should you notice any changes in your skin, such as symptoms suggestive of seborrheic dermatitis.
 Monica Enamandram, M.D. is a resident physician at Memorial Sloan-Kettering Cancer Center. She earned her MD degree at Harvard Medical School, and will continue her residency training in Dermatology at Stanford University Hospitals. She is interested in patient education and clinical research in dermatology, and is excited to develop successful preventive measures and treatment regimens for eczema.
Monica Enamandram, M.D. is a resident physician at Memorial Sloan-Kettering Cancer Center. She earned her MD degree at Harvard Medical School, and will continue her residency training in Dermatology at Stanford University Hospitals. She is interested in patient education and clinical research in dermatology, and is excited to develop successful preventive measures and treatment regimens for eczema.